Feeding Tube Insertion (Gastrostomy)
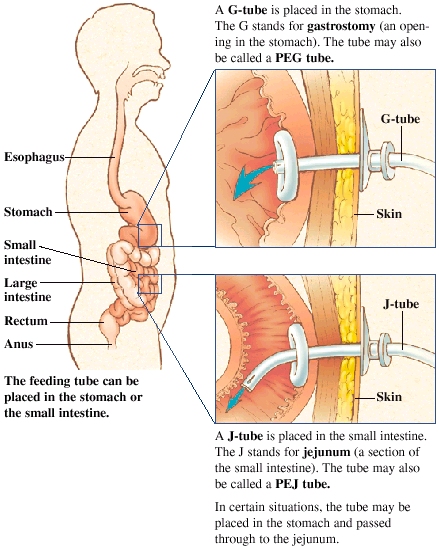
A G-tube is placed in the stomach. The G stands for gastrostomy (an opening in the stomach). The tube may also be called a PEG tube. Percutaneous endoscopic gastrostomy (PEG), esophagogastroduodenoscopy (EGD), and G-tube insertion.
A J-tube is placed in the small intestine. The J stands for jejunum ( a section of the small intestine). The tube may also be called a PEJ tube.
In certain situations, the tube may be placed in the stomach and passed through to the jejunum.
What Is a Feeding Tube?




Gastrostomy may be indicated in numerous situations, usually those in which normal or nutrition (or nasogastric) feeding is impossible. The causes for these situations may be neurological (e.g. stroke), anatomical (e.g. cleft lip and palate during the process of correction) or other (e.g. radiation therapy for tumors in head & neck region).
In certain situations where normal or nasogastric feeding is not possible, gastrostomy may be of no clinical benefit. In advanced dementia, studies show that PEG placement does not in fact prolong life. Instead, oral assisted feedings are preferable. Quality improvement protocols have been developed with the aim of reducing the number of non-beneficial gastrostomies in patients with dementia.
A gastrostomy can be placed to decompress the stomach contents in a patient with a malignant bowel obstruction. This is referred to as a "venting PEG" and is placed to prevent and manage nausea and vomiting.
A gastrostomy can also be used to treat volvulus of the stomach, where the stomach twists along one of its axes. The tube (or multiple tubes) is used for gastropexy, or adhering the stomach to the abdominal wall, preventing twisting of the stomach.
A PEG tube can be used in providing gastric or post-surgical drainage.
The Gauderer-Ponsky technique involves performing a gastroscopy to evaluate the anatomy of the stomach. The anterior stomach wall is identified and techniques are used to ensure that there is no organ between the wall and the skin:
In the Russell introducer technique, the Seldinger technique is used to place a wire into the stomach, and a series of dilators are used to increase the size of the gastrostomy. The tube is then pushed in over the wire.
PEG tubes with a collapsible or deflatable bumper can be removed using traction (simply by pulling the PEG tube out through the abdominal wall).
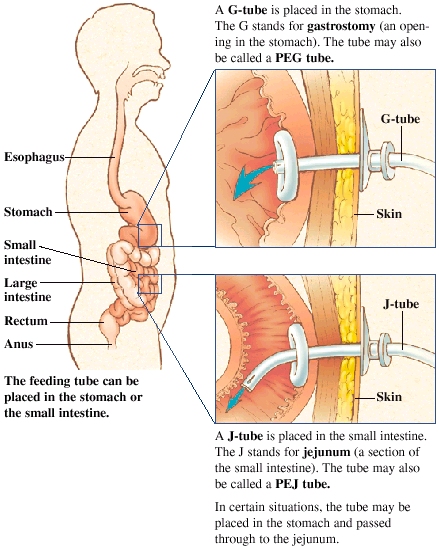
A G-tube is placed in the stomach. The G stands for gastrostomy (an opening in the stomach). The tube may also be called a PEG tube. Percutaneous endoscopic gastrostomy (PEG), esophagogastroduodenoscopy (EGD), and G-tube insertion.
A J-tube is placed in the small intestine. The J stands for jejunum ( a section of the small intestine). The tube may also be called a PEJ tube.
In certain situations, the tube may be placed in the stomach and passed through to the jejunum.
What Is a Feeding Tube?
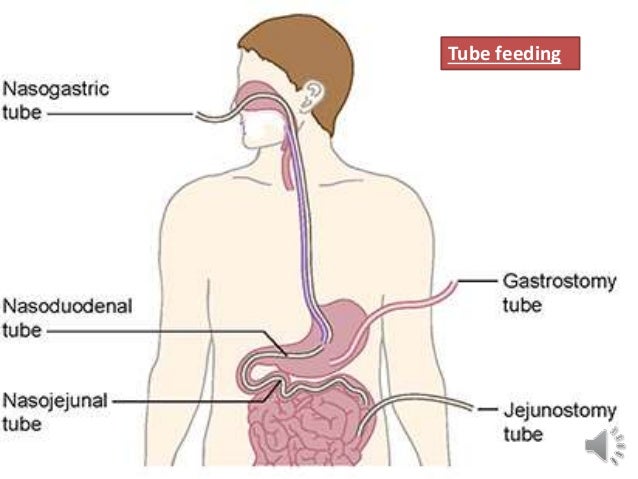
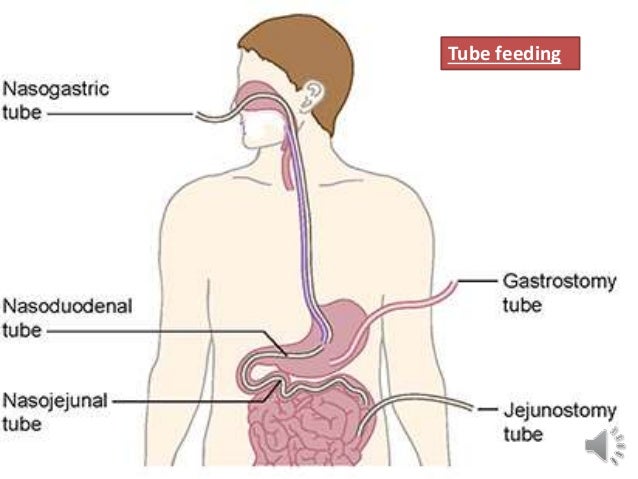
A feeding tube is a device that’s inserted into your stomach through your abdomen. It’s used to supply nutrition when you have trouble eating. It’s also called percutaneous endoscopic gastrostomy (PEG), esophagogastroduodenoscopy (EGD), and G-tube insertion.
This treatment is reserved for when you have trouble eating on your own. This can be because:
- you have a deformity of your mouth or esophagus, which is the tube that connects your throat to your stomach
- you have difficulty swallowing or keeping food down
- you aren’t getting enough nutrition or fluids by mouth
The treatment can also done if you need it to receive certain medications.
Preparation
Do I Need to Prepare for the Procedure?
This procedure is performed in a hospital or clinic. Before you begin, tell your doctor about any medications you’re taking, including blood thinners such as warfarin (Coumadin), aspirin, or clopidogrel (Plavix). You’ll need to stop taking blood thinners or anti-inflammatory medications one week or so before the procedure. Your doctor will also need to know if you have certain conditions such as:
- pregnancy
- diabetes
- allergies
- heart conditions
- lung conditions
If you have diabetes, your oral medications or insulin may have to be adjusted the day of the procedure.
Your doctor will perform a gastrostomy using an endoscope, which is a flexible tube with a camera attached. You may be given anesthesia to make you more comfortable. This may make you drowsy following the procedure. Arrange before the procedure to have someone available to drive you home.
This procedure requires you to fast. Typically, doctors ask that you abstain from eating eight hours before the procedure. Most people can return home the same day as the procedure or the following day.
Procedure
How Is the Endoscope Inserted?
During the procedure, you’ll be asked to remove any jewelry or dentures. You’ll then be given an anesthetic and something to relieve the pain. You’ll lie on your back. Your doctor will place the endoscope in your mouth and down your esophagus. The camera will help the doctor visualize your stomach lining to ensure that the feeding tube is positioned properly.
When your doctor can see your stomach, they’ll make a small incision in your abdomen. Next, they’ll insert the feeding tube through the opening. They will secure the tube and place a sterile dressing around the site. There may be a little drainage of bodily fluids, such as blood or pus, from the wound. The whole procedure usually lasts less than an hour.
The feeding tube can be temporary or permanent, depending on the primary reason for the feeding tube.
After the Procedure
The medicine may make you drowsy. Plan on resting after the procedure. Your abdomen should heal in about five to seven days. After the tube is inserted, you may meet with a dietician who will show you how to use the tube for feeding. Your dietician will also educate you on how to care for the tube.
Drainage around the tube is normal for a day or two, and a nurse will probably change your dressing on a regular basis. Feeling pain for a few days around the place where the incision was made is normal. Make sure to keep the area dry and clean to avoid skin irritation or infection.
There are some risks associated with the procedure, but they aren’t common. Risks include trouble breathing and nausea from the medication. Excessive bleeding and infection are risks whenever you have surgery, even with a minor procedure such as a feeding tube insertion.
When to Call the Doctor
Before you leave the hospital or clinic, make sure you know how to care for your feeding tube and when you need to contact a doctor. You should call your doctor if:
- the tube comes out
- you have trouble with the formula or if the tube becomes blocked
- you notice bleeding around the tube insertion site
- you have drainage around the site after several days
- you have signs and symptoms of an infection, including redness, swelling, or a fever
Gastrostomy may be indicated in numerous situations, usually those in which normal or nutrition (or nasogastric) feeding is impossible. The causes for these situations may be neurological (e.g. stroke), anatomical (e.g. cleft lip and palate during the process of correction) or other (e.g. radiation therapy for tumors in head & neck region).
In certain situations where normal or nasogastric feeding is not possible, gastrostomy may be of no clinical benefit. In advanced dementia, studies show that PEG placement does not in fact prolong life. Instead, oral assisted feedings are preferable. Quality improvement protocols have been developed with the aim of reducing the number of non-beneficial gastrostomies in patients with dementia.
A gastrostomy can be placed to decompress the stomach contents in a patient with a malignant bowel obstruction. This is referred to as a "venting PEG" and is placed to prevent and manage nausea and vomiting.
A gastrostomy can also be used to treat volvulus of the stomach, where the stomach twists along one of its axes. The tube (or multiple tubes) is used for gastropexy, or adhering the stomach to the abdominal wall, preventing twisting of the stomach.
A PEG tube can be used in providing gastric or post-surgical drainage.
Techniques
Two major techniques for placing PEGs have been described in the literature.The Gauderer-Ponsky technique involves performing a gastroscopy to evaluate the anatomy of the stomach. The anterior stomach wall is identified and techniques are used to ensure that there is no organ between the wall and the skin:
- digital pressure is applied to the abdominal wall, which can be seen indenting the anterior gastric wall by the endoscopist.
- transillumination (diaphanoscopy): the light emitted from the endoscope within the stomach can be seen through the abdominal wall.
- a small (21G, 40mm) needle is passed into the stomach before the larger cannula is passed.
In the Russell introducer technique, the Seldinger technique is used to place a wire into the stomach, and a series of dilators are used to increase the size of the gastrostomy. The tube is then pushed in over the wire.
Contraindications
As with other types of feeding tubes, care must be made to place PEGs into an appropriate population. The following are contraindications to PEG use:Absolute contraindications
- Inability to perform an esophagogastroduodenoscopy
- Uncorrected coagulopathy
- Peritonitis
- Untreatable (loculated) massive ascites
- Bowel obstruction (unless the PEG is sited to provide drainage)
Relative contraindications
- Massive ascites
- Gastric mucosal abnormalities: large gastric varices, portal hypertensive gastropathy
- Previous abdominal surgery, including previous partial gastrectomy: increased risk of organs interposed between gastric wall and abdominal wall
- Morbid obesity: difficulties in locating stomach position by digital indentation of stomach and transillumination
- Gastric wall neoplasm
- Abdominal wall infection: increased risk of infection of PEG site
- Intra-abdmominal malignancy with peritoneal involvement (tumor seeding into formed channel with subsequent failure)
In advanced dementia
The American Medical Directors Association, the American Geriatrics Society and the American Academy of Hospice and Palliative Medicine recommend against inserting percutaneous feeding tubes in individuals with advanced dementia and, instead, recommend oral assisted feedings. Artificial nutrition neither prolongs life nor improves its quality in patients with advanced dementia. It may increase the risk of the patient inhaling food, it does not reduce suffering, it may cause fluid overload, diarrhea, abdominal pain and local complications, and can reduce the amount of human interaction the patient experiences.[Complications
- Cellulitis (infection of the skin) around the gastrostomy site
- Hemorrhage
- Gastric ulcer either at the site of the button or on the opposite wall of the stomach ("kissing ulcer")
- Perforation of bowel (most commonly transverse colon) leading to peritonitis
- Puncture of the left lobe of the liver leading to liver capsule pain
- Gastrocolic fistula: this may be suspected if diarrhea appears a short time after feeding. In this case, the feed goes direct from stomach to colon (usually transverse colon)
- Gastric separation
- "Buried bumper syndrome" (the gastric part of the tube migrates into the gastric wall)
Removal of PEG tubes
Indications
- PEG tube no longer required (recovery of swallow after stroke or brain trauma, or after surgery or radiotherapy for head and neck cancer)
- Persistent infection of PEG site
- Failure, breakage or deterioration of PEG tube (a new tube can be sited along the existing track)
- "Buried bumper syndrome"
Techniques
PEG tubes with rigid, fixed "bumpers" are removed endoscopically. The PEG tube is pushed into the stomach so that part of the tube is visible behind the bumper. An endoscopy snare is then passed through the endoscope, and passed over the bumper so that the tube adjacent to the bumper is grasped. The external part of the tube is then cut, and the tube is withdrawn into the stomach, and then pulled up into the esophagus and removed through the mouth. The PEG site heals without intervention.PEG tubes with a collapsible or deflatable bumper can be removed using traction (simply by pulling the PEG tube out through the abdominal wall).


Hey, I even have looking your article and that helped me to put in writing my article about honeycrisp apple nutrition facts you want to have a test on my article.
ReplyDelete