Influence of age on thirst and fluid intake
W. LARRY KENNEY and PERCY CHIU
Noll Physiological Research Center and Schreyer Honors College, Penn State University, University Park, PA 16802
ABSTRACT
KENNEY, W. L., and P. CHIU.
Influence of age on thirst and fluid intake.
Med. Sci. Sports Exerc., Vol. 33, No. 9, 2001, pp.1524–1532. Independently living older adults (over the age of 65 yr) consume adequate volumes of fluids on a daily basis. However,when challenged by fluid deprivation, a hyperosmotic stimulus, or exercise in a warm environment (all of which combine hypovolemia and hyperosmolality), older adults exhibit decreased thirst sensation and reduced fluid intake. Full fluid restoration eventually occurs, but full restoration of fluid balance is slowed. The aging process alters important physiological control systems associated with thirst and satiety. Recent evidence suggests that older men and women (i) have a higher baseline osmolality and thus a higher osmotic operating point for thirst sensation (with little or no change in sensitivity), and (ii) exhibit diminished thirst and satiety in response to the unloading (hypovolemia) and loading (hypervolemia) of baroreceptors. A diminished sensation of thirst in the elderly relative to young adults is generally absent when a volume stimulus is absent, despite higher baseline plasma osmolalities. Compared with the elderly, there are scant data associated with homeostatic control of thirst in children. Non homeostatic control of thirst and drinking behavior may likewise be different for children (as it is for the elderly), as compared with young adults; however, little empirical data exist on this topic. Children rarely exhibit voluntary dehydration for activities lasting 45 min or less; however, drink flavoring and sodium chloride are important promoters of drinking in active children.
Key Words: AGING, DRINKING BEHAVIOR, CHILDREN,ELDERLY, OSMOLALITY, BLOOD VOLUME, HYDRATION, DEHYDRATION.
[Osmolality of blood increases with dehydration and decreases with over hydration. In normal people, increased osmolality in the blood will stimulate secretion of antidiuretic hormone (ADH). This will result in increased water reabsorption, more concentrated urine, and less concentrated blood plasma.] [Read about "Plasma osmolality" click here]
The health benefits of proper hydration have long been recognized, both regular daily hydration (unchallenged) and in response to dehydration (the process by which an acute fluid deficit occurs) or hypo-hydration (the term that connotes the level of fluid deficit). A major component of this rehydration process involves thirst which—depending on drink availability—leads to voluntary fluid intake. The manifestations of thirst have been characterized as a combination of sensations that increase with dehydration and decrease with rehydration (restoration of fluid balance), including a dry, scratchy mouth and throat,chapped and dry lips, light-headedness, dizziness, tiredness,irritability, headache, loss of appetite, and feeling of an“empty stomach” (24).
FIGURE 1—Homeostatic versus nonhomeostatic control of thirst in humans. Under stressed (dehydrated) conditions, thirst results from increases in cellular tonicity and decreases in extracellular volume. Nonhomeostatic controls include a variety of influences, including—but not limited to—those shown here.
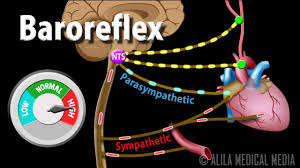
Thirst results from a complex interaction of physiological control systems and behavioral influences. Figure 1 shows the distinction between physiologically determined thirst and drinking behavior that is under the influence of non homeostatic control. Physiological thirst results from dehydration (no further distinction will be made here between dehydration and hypo-hydration) and is stimulated by two main homeostatic mechanisms: increases in cellular tonicity (cellular dehydration) and decreases in extracellular fluid volume (extracellular dehydration). The former is sensed by osmoreceptors in the central nervous system, whereas the latter is monitored by baroreceptors in the vascular compartment. Since dehydration causes fluid losses from the intracellular and extracellular spaces, redundant sensing for the purposes of fluid balance decreases the likelihood of error in these feedback loops.
Cellular dehydration is an important thirst stimulus in humans. Drinking is stimulated by increases in the effective osmotic pressure of the plasma. Central (and possibly peripheral) osmoreceptors sense the level of dehydration and feed back to the hypothalamus to maintain homeostasis. In animal models, thirst depends on a tonicity sensor that is located outside the blood-brain barrier, possibly in one of the circumventricular* organs of the brain (30).[*Circumventricular organs (CVOs) are structures in the brain that are characterized by their extensive vasculature and lack of a normal blood brain barrier (BBB). ] Localization of primary osmosensing organ(s) is lacking in humans, but it is likely also located in this region. Depending on these osmoreceptors, thirst thresholds are set and thirst is stimulated on the basis presumably of an error signal (i.e., the deviation of the sensed plasma osmolality from some “normal” operating point). This system has been modeled as a single feedback loop (35) as depicted in the left portion of Figure 2.
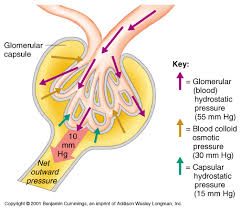
Extracellular dehydration as a thirst stimulus is more complex, as depicted on the right-hand side of Figure 2. This double feedback loop involves both baroreceptors in large vessels, which are activated with decreases in blood volume,and renal mechanisms, which elicit the renin-angiotensin-aldosterone system in response to decreased renal perfusion and other stimuli. Hormonal activation of a salt appetite(more well defined in animal models than in humans) adds to the complexity of both volume and osmo regulation of thirst (Fig. 2). This mechanism, however, has been suggested to be the less predominant of the two in young adults,and it has been suggested that decreased extracellular volume becomes a fundamental thirst stimulus only in cases of severe dehydration (29). However, as discussed later in this article, strong data to the contrary exist (e.g., Stachenfeld etal. (33)). The relative influences of intra- and extracellular dehydration in children is undetermined. In the elderly, a clearer picture is beginning to emerge with respect to these mechanisms. In general, although regulation of the physio-logical thirst mechanism has long been studied in young adults, many important questions remain with respect to differences in thirst sensation and fluid intake in children and the elderly.
A third mechanism that helps regulate thirst also deserves mention. In humans, the act of swallowing helps to regulate the volume of fluid ingested by providing an integrated signal proportional to the cumulative ingested volume(termed “oropharyngeal metering”). Figaro and Mack (10)dehydrated six subjects by light exercise in a warm environment on three different occasions (⫺28.6 mL·kg power to minus1 body-weight (BW)). Rehydration involved one of three treatments(all occurring with a nasogastric (NG) feeding tube insert-ed). The first involved 75 min of ad libitum drinking (which averaged 20.0 plus-minus 2.0 mL·kg (power to the minus 1) BW). The second rehydration treatment involved the infusion of an identical volume directly into the stomach via the NG tube plus ad libitum drinking after 25 min. The third treatment involved ad libitum drinking again, but with immediate withdrawal of the fluid from the stomach. Reflex inhibition of thirst began within 5 min of rehydration in groups 1 and 3, but not in the infusion group. Ad libitum drinking without absorption(withdrawn with NG tube) resulted in only 15% more fluid intake than the ad libitum condition. These data demonstrate a clear role of esophageal metering in determining fluid intake during dipsogenic stimuli in humans.
In addition to the homeostatic mechanisms mentioned above, there are also myriad non homeostatic controls that add to the stimulation of thirst. These include a wide array of psychological and environmental influences such as availability of the beverage; taste, temperature, and palatability of the beverage; knowledge about the importance of proper hydration; drinking in association with meals; social and societal norms and habits; and even the presence of others who are consuming a beverage. Ad libitum drinking is typically done in association with meals. When a variety of foods and drinks are available, spontaneous drinking occurs and exceeds the volume necessary for fluid balance(29), with excess fluid eliminated by the kidneys. This is true not only for young adults but also for children and for healthy independently living older adults (8). Given free access to fluid, humans become thirsty and drink before body fluid deficits appear, perhaps in response to subtle oropharyngeal cues or simply because of habit or social norm (29). Undoubtedly, such behavioral cues are different in children and in the elderly, but little research has been performed in this important area.
EXPERIMENTAL THIRST STIMULATION
Most laboratory and field studies of thirst have invoked a dehydrating stimulus such as restricted access to fluid in-take, prolonged dynamic exercise (often performed in a warm environment), or infusion of hypertonic saline. Such studies then allow unrestricted access to monitored fluids during a rehydration period after dehydration, or the subjects are allowed unrestricted access to monitored fluids throughout a multi day trial. Table 1 lists several types of the various perturbations that have been used in published studies on older adults. Fluid deprivation and exercise both create a hypovolemic, hyperosmotic condition, the most common milieu associated with dehydration. Hypertonic saline infusion can provide either a relatively euvolemic or hypervolemic hyperosmotic condition, depending on the volume and tonicity of the infusate. And finally, drives for thirst and for satiety can be provided simultaneously in the laboratory, for example, by head-out water immersion ...
[FIGURE 1—Homeostatic versus non homeostatic control of thirst in humans. Under stressed (dehydrated) conditions, thirst results from increases in cellular tonicity and decreases in extracellular volume. Non homeostatic controls include a variety of influences, including—but not limited to—those shown here.]
[FIGURE 2—Simplified model for homeostatic control of thirst showing feedback loops and redundancy (redrawn from Stricker and Verbalis (35)). Osmoregulatory thirst is a single feedback loop with correction proceeding until the dehydration is corrected. Hypovolemic thirst is modeled as a double-loop negative feedback system in which water alone cannot correct the plasma volume deficit. Therefore, water intake is not maintained despite the presence of a hypovolemic stimulus. Sodium intake serves to expand plasma volume and to avoid excess osmotic dilution.]
... immediately following dehydration (33). Although such experiments have yielded important data for older adults, no such data exist for children.
TABLE 1. Summarized studies of various laboratory methods of thirst stimulation in older adults according to the stimulus used to evoke thirst.
Perturbation ↑O ↓V Effect on Thirst (Relative to Young Subjects), Study (Reference)
1.Fluid restriction ↑ ↓ Decreased thirst and fluid intake for a given weight loss, Phillips and Roll (25)
2.Exercise in the heat ↑ ↓ Decreased thirst ratings; fluid intake matched thirst ratings; osmolality threshold elevated and sensitivity reduced, Mack et al. (15)
3.Passive prolonged heat stress ↑ ↓ Decreased thirst ratings but similar fluid intakes, Miescher and Fortney (19)
4.Hypertonic saline infusion ↑ ( Decreased thirst ratings, Phillips et al. (21)
5.Hypertonic saline infusion ↑ (↓) Similar thirst ratings; similar plasma arginine response, Stachenfeld et al. (34)
6.Exercise in the heat; head-out immersion ↑ (↓) Decreased thirst before immersion; restoration of central volume reduced thirst and drinking only in young subjects, Stachenfeld et al. (33)
7.Thirst suppression by fluid loading (↓) (↑) Thirst blunted in young subjects only, Crowe et al. (5) and Phillipset al. (22)
8.Exercise-heat acclimation ↑ ↓ Decreased fluid intake in older subjects during recovery from daily exercise (6 d) led to inability to expand plasma volume, Takamata et al. (36)
9.Exercise-heat acclimation ↑ ↓ Decreased daily fluid intake in older subjects over a 4-d exercise period led to inability to expand plasma volume, Zappe et al. (39)
Body weight before and after experiments, plasma volume, and plasma osmolality measurements are typically the dependent variables used to assess rehydration efficacy.However, visual analog scales of thirst ratings and questionnaires are still the standard methods used to quantify thirst. Reliable and valid use of subjective scales may be problematic for children and some elderly subjects. Further-more, several discrepancies appear in the literature with respect to thirst ratings under “baseline euhydrated” conditions (e.g., Mack et al. (15)).
RESEARCH REVIEW
Older Adults
The gerontology literature contains multiple reports of altered hydration status in the elderly. Careful reading suggests that most of this information comes from anecdotal evidence and facts extrapolated from clinical and institutionalized older populations. For example, in one study,dehydration was evident in about 25% of non ambulatory geriatric hospital patients (32). Another article reported that a majority of patients over age 65 from six continuing care hospital wards had elevated serum osmolalities (>296mOsm·kg to the power minus1), and a group of 58 patients randomly selected had a mean plasma osmolality of 304 plus-minus 8 mOsm·kg to the power minus1 at time of hospital admission (20). As further evidence of a problem with hydration in the elderly, a common textbook observation is that when older patients are hospitalized,many cannot or will not spontaneously ask for fluids (1).Extrapolating such statistics to non institutionalized, healthy older men and women leads to the inaccurate conclusion that many older individuals walk around in a frank state of hyperosmolar hypo-hydration. This does not appear to be the case.
Despite the statistics cited above for geriatric hospitals,dehydration is evident in only about 1% of older patients admitted to community hospitals, a better indicator of the health status of independently living adults (31). Even in the hyperosmolar institutionalized patients surveyed by O’Neillet al. (20) (ages 67–101 yr), there was no correlation be-tween age and osmolality. Therefore, it is more plausible that dehydration in the elderly (i) accompanies, or results from, various clinical conditions and/or medications, or (ii)reflects an age-specific response to mild water deprivation(discussed in detail below). Both the incidence and the magnitude of chronic dehydration in the healthy community-dwelling older adult are overstated. However, to err on the side of safety, proper hydration practices during high-risk times (e.g., projected heat waves, long duration activity in hot environments) should be taught and fluid intake should be emphasized in this population.Spontaneous fluid ingestion by healthy older adults. Do older men and women, on a day-to-day basis,consume less fluid than younger men and women? What dictates spontaneous ad libitum fluid intake, and do those stimuli change as we age? Under ad libitum conditions, in natural environments, neither the amount nor the pattern of fluid intake is regulated physiologically to any great extent(6,25). Rather, both are governed by the amount and timing of food intake (6,7,25). Enough fluid is consumed with meals to maintain adequate fluid balance, and under unstressed conditions the renal response is sufficient to maintain this balance.
This concept seems to apply to the older adult population as well. When fluids are readily available, independently living healthy older individuals have daily fluid intakes that are similar to those of younger individuals. In one study, 262 adults aged 20–80 yr were asked to maintain a food and fluid intake diary for 7 consecutive days. There were no notable age differences in total fluid intake (food water content plus fluids drunk), water intake in excess of that required for digestion (“surplus water”), or overall volume of fluid consumed. Nor was there an age effect for thirst, its relationship to fluid intake, or the amount of fluid ingested relative to the amount of solids ingested during a meal (8).Even in those few surveys of community-dwelling older men and women that report slight reductions of fluid intake,their intake is not substantially reduced. In a Dutch survey of 539 healthy, independently living adults aged 65–79 yr,daily water intake averaged 2.15 L·d⫺1for men and 1.98L·d⫺1for women. Although the nonalcoholic beverage in-take of the 75- to 79-yr-old group was lower than that of younger subjects, even the lowest daily intake reported(1.87 L·d⫺1) was well within what the authors considered the normal range of 1.6–2.4 L·d⫺1(14). However, it is important to realize, as pointed out by Rolls (29), that if older individuals do not feel well or if access to palatable fluids is in any way restricted, problems may develop.
Thus, enough fluid is consumed in response to non regulatory stimuli (i.e., with meals) to maintain adequate fluid balance, and under unstressful conditions the kidney response of older persons is sufficient to maintain this balance. Therefore, afferent physiological signals that arise from a fluid deficit are rarely produced, and physiologically mediated mechanisms are seldom called on under conditions of normal daily life (8). This may be especially true for the older adult population, which as a population tends toward a more sedentary lifestyle.
“Baseline” osmolality, plasma volume, and euhydration in the elderly. On the surface, it seems difficult to reconcile the above discussion with data from several laboratory studies. When older subjects report for laboratory studies designed to challenge fluid balance, they are typically in a normal state of hydration (5,12,35), but an elevated plasma osmolality (typically by about 3– 6m Osm·kg to the power minus1) is often noted in these older subject groups at“baseline” (5,9,15,19). Such small differences in blood tonicity have led to the conclusion that “healthy, active older[individuals] are hyperosmotic and hypovolemic” (15).However, such studies typically require an overnight fast without pre experimental fluid intake; thus, the “baseline”plasma variables that are reported in some studies may actually reflect a dehydrated state. An overnight fast should more accurately be viewed as a mild dehydration, which may selectively render older subjects slightly hyperosmotic and hypovolemic if renal function is altered. This is clearly not the entire reason for elevated plasma osmolalities in older subjects, since differences are seen even in studies where pre-exercise fluid intake is standardized (15). Further-more, when older and younger subjects are matched for maximal aerobic capacity and body composition, baseline differences in both plasma osmolality and plasma volumeare minimized (12). Because the elevated osmolality of older men and women is not associated with elevated plasma sodium concentrations, it may better reflect elevations in substances like glucose and blood urea nitrogen.
Dehydration and aging: non thirst factors. Voluntary fluid intake after dehydration is clearly influenced by non thirst factors such as the availability of fluids and their palatability. Although thirst and volume of fluid ingested are separate entities, they seem to be affected in parallel by age,and increasing the availability or palatability of fluids does not seem to significantly increase water deprivation-induced fluid intake in older men and women (23). After two separate bouts of dehydration (fluid deprivation plus a dry diet),healthy older men were offered either water, mineral water,or a variety of other palatable beverages, including cola and orange juice (23). Orange juice was consumed in larger volumes on single occasions, suggesting a higher palatability, yet over a 2-h period there was no difference in fluid consumption between trials or beverages. Although these results imply that palatability alone is insufficient to over-come the reduced thirst sensation associated with aging, the tonicity of the fluid consumed may be important in the time course of drinking (11) and in the effectiveness of re-hydration (22).
Aging and thirst. Under normal conditions of daily living, increased thirst and fluid intake defend against any threats to fluid homeostasis that may result from altered free-water clearance by the kidneys. Therefore, although an inadequate renal response to mild water deprivation may play a role in any fluid volume depletion occurring in older persons, reduced thirst is probably more important (22). Ad libitum fluid intake can be directly measured, but thirst is typically assessed using visual analog scales involving questions such as, “How thirsty do you feel now?” Care should be taken to ensure that older subjects interpret such scales and rate their thirst sensations in a manner similar to younger subjects.
As shown in Figures 1 and 2, thirst can be elicited by situations or manipulations that decrease extracellular fluid volume, increase intracellular tonicity, or both. Most natural situations, such as exercise, exogenous heat stress, and fluid deprivation, simultaneously decrease volume and increase tonicity. After a 24-h period of restricted water intake that caused an equal weight loss in older and younger subjects,a group of healthy men 67–75 yr old were less thirsty and replaced less of the fluid deficit over the next 2 h than did young controls (26). This initial finding of reduced thirst with advancing age has been confirmed using exercise/heatstress to induce both a volume deficit and hyperosmolality(15). Additionally, Mack et al. (15) showed that the relationship between thirst rating and fluid intake was not altered by age. Conversely, data from Miescher and Fortney(19) dissociated thirst ratings from fluid intake in older men after a prolonged passive heat stress; that is, the older men were thirstier but drank the same volume of water. When both volume and tonicity are affected by dehydration, older individuals operate around a higher plasma osmolality (a shift in the operating point of the system) and on a less steep portion of the stimulus-response curve (15).
Volume or osmolality deficit? Since either hypovolemia or hypertonicity can independently cause sensations of thirst, a compelling question is whether one of these control loops (depicted in Fig. 2) is significantly altered by the aging process, or whether both are impaired. Table 1 presents a variety of studies that independently or simultaneously decreased intravascular volume or increased plasma osmolality. Infusion of hypertonic saline has been used to increase osmolality (and create an osmotic thirst drive)while increasing plasma volume (i.e., creating a hyperosmolar hypervolemia). Phillips et al. (21) infused hypertonic saline (0.855 M) over a 2-h period in older and younger men. Although both age groups experienced an increased thirst sensation and water intake, the older men reported feeling less thirsty and drank less room-temperature water.Alternately, when Stachenfeld et al. (34) performed a similar study, osmotically stimulated increases in thirst were unaffected by age. Three methodological differences should be noted between these two studies. In the study by Phillipset al., subjects appeared at the laboratory after an overnight
fast, whereas the subjects in the study by Stachenfeld et al. ate a light breakfast and drank ~5 mL·kg⫺1 of water 1 hour before the experiment. Neither study reported a baseline difference in plasma osmolality between age groups. Second, Stachenfeld and colleagues infused 40% more saline(although the sodium load was similar), raising PV by 16–18% in both age groups. Phillips caused a significant PV expansion (by 9%) in the young men only. Finally, and perhaps most importantly, subjects were tested supine by Phillips et al. and upright by Stachenfeld et al. Therefore, in the former, baroreceptors were unloaded before the saline infusion.
Figure 3 is presented to help clarify the complex question of hyperosmolar thirst and aging. Under “normal daily”conditions, baseline differences in osmolality—in the presence of a lower plasma volume (Fig. 3a and b)—appear to shift the operating point for osmotic thirst to the right in older subjects. Although the baseline (shown by the circled points) is shifted rightward, no data exist that demonstrate a true shift in the operating point (i.e., a steady state condition with some point above which deviation from baseline oc-curs). However, when the baseline is similar and volume is expanded in both age groups (Fig. 3c), no difference is noted. Therefore, in young adults, thirst is greater at a given plasma osmolality during dehydration because of the hypovolemic stimulus, and the thirst response is attenuated at any given plasma osmolality during saline infusion because of the relative hypervolemia (34). Older individuals appear to be as sensitive to increased tonicity but less sensitive to volume changes. The rightward shift in Figure 3 may reflect the inability of older subjects to shift the response leftward with dehydration in the absence of volume expansion.
Age and thirst suppression. The inverse of causing thirst by fluid deprivation is blunting thirst by oral fluid loading or expansion of (or a central shift in) blood volume. Crowe et al. (5) found that after young adults ingested 20mL·kg to the power of minus 1 water loads, thirst was suppressed for 1–2 hours and then increased progressively over the following 5–6 hours,whether they were initially fluid-depleted or not. Conversely, water-replete older men (mean age, 72 yr) showed no alteration in their thirst ratings over the entire 7 h after the water loads, despite clear indications that an osmotic thirst stimulus had occurred. Phillips et al. (22) also studied water-deprived (24 h) older and young men. Although thirst increased after water deprivation in both groups, it increased less in the elderly. When oral water loads of 10 mL·kg⫺1were subsequently given over a 2- to 3-min period, thirst was suppressed in both age groups; however, plasma AVP fell immediately after drinking only in the young group.These results demonstrate reduced oropharyngeal inhibition of AVP secretion in healthy older men despite maintained inhibition of thirst.
More recently, Stachenfeld et al. (33) used a novel experimental design to test the influence of central blood volume on thirst. After older and younger adults dehydrated by overnight water restriction and subsequent exercise in the heat, they recovered with or without head-out immersion(HOI). HOI forces blood volume centrally, loading baroreceptors and mimicking hypervolemia (or in this case, minimizing hypovolemia). In the young subjects, HOI caused an immediate fall in thirst perception and a dramatic reduction in ad libitum fluid intake (Fig. 4).
A similar central blood volume expansion had no effect on thirst in the older subjects, however. Figure 5 presents a model for the foregoing discussion and conclusion.
It appears that when the sole stimulus for thirst and drinking is osmotic, there is little difference in thirst sensation in older adults compared with their younger counterparts. A deficit in the sensitivity of volume receptors appears to be a more important mechanism accounting for reduced thirst with aging.
Thirst during repeated exposures (acclimation). Body fluid regulation is influenced by acclimation status. In young adults, repeated bouts of exercise in hot environments results in an expansion of plasma volume primarily because of increased voluntary fluid intake (39). Zappe and colleagues (39) exercised young and older (67 plus-minus 1 yr old) adults in a 30°C environment for 4 consecutive days while monitoring PV, renal function, and daily 24-h fluid intake(Fig. 6c–e). Whereas the young subjects increased PV by10%, the older men did not expand their plasma volume significantly. This failure to increase intravascular volume was not caused by impaired renal water conservation but ...
[ FIGURE 3—Data are shown from three published studies (15,36,34) in which thirst ratings (standardized here as percentage of the full visual analog scale used to rate thirst subjectively) were plotted against plasma osmolality. Solid arrows connect pre-dehydration and post-dehydration data for young subjects in each panel; dashed arrows connect data points for older subjects. Baseline data points in each age group and experiment are circled.Panels a and b involved thermal dehydration, and baseline age differences were present for plasma volume and plasma osmolality. When there was no age difference in plasma volume (panel c; hypertonic saline infusion) and volume was expanded in both age groups, osmolar regulation of thirst was not different between young and older men. The authors speculated that plasma volume expansion modulated thirst in young, but not in older, subjects. See Figure 5 also.]
... rather by a smaller increase in 24-h fluid intake, which averaged 32 mL·kg to the power minus1·d to the power minus1in the older men versus 45mL·kg to the power minus1·d to the power minus1 in the younger men. These findings were later confirmed during a 6-d heat acclimation protocol (36) (Fig.6a and b).
After daily low-intensity intermittent exercise for 6 d,young men expanded PV by 5%, whereas the older men did not. During a 2-h recovery period after each exercise session, young men replaced, on average, 80% of lost fluid drinking a carbohydrate-electrolyte drink, compared with 34% fractional fluid recovery in the 70-yr-old group. This greater involuntary dehydration was accompanied by reduced thirst ratings, lower plasma vasopressin and aldosterone concentrations, and less renin activity. The plasma osmolality-thirst relationship was shifted rightward in the older subjects, i.e., a higher baseline plasma osmolality and elevated osmolar thirst threshold (pre-acclimation data are shown in Fig. 3b). However, the acclimation protocol had little effect on osmo-regulation of thirst, leading the authors to implicate attenuated baroreflex* (volume) control.
[*The baroreflex provides a rapid negative feedback loop in which an elevated blood pressure reflexively causes the heart rate to decrease and also causes blood pressure to decrease. Decreased blood pressure decreases baroreflex activation and causes heart rate to increase and to restore blood pressure levels. ]
They speculated that the older men may have had a lower baroreflex sensitivity and the acclimation program did not further attenuate this sensitivity, thus fluid intake was not altered.
Conclusion. When challenged by fluid deprivation, a hyperosmotic stimulus, hypovolemia, or exercise in a warm environment, older adults exhibit a decreased thirst sensation and reduced fluid intake. Acutely, fluid restoration is eventually effective, but restoration of fluid balance is slower. Longer term fluid intake (i.e., days to weeks) in
[FIGURE 6—A critical component of heat acclimation is the expansion of plasma volume during the first 2–5 days.
This involves increased fluid intake and increased plasma protein translocation. Data from Takamata et al. (36) (panels a and b) and Zappe et al. (39) (panels c–e) show that plasma volume expansion is attenuated in older subjects, as is post exercise fluid intake and daily fluid intake during the initial acclimation stage.]
[ FIGURE 4—When older (70 2 yr) and young (24 ⴞ 1 yr) subjects undergo dehydration, the sensation of thirst increases to a greater extent in the young subjects. When central fluid volume is restored acutely by head-out immersion, thirst is attenuated in young subjects only, even though 70% of the plasma volume loss was restored in the older men. This suggests that age differences in thirst arise from changes in the cardiovascular system (i.e., baroreceptor function or responsiveness). In both age groups, fluid intake followed thirst ratings. (Data redrawn from Stachenfeld et al. (33).)]
[ FIGURE 5—A unifying hypothesis proposed by Stachenfeld et al. (33) to explain differences in thirst between older and younger adults. During “normally occurring” dehydration, osmolality increases and blood volume decreases. Young adults are thirstier at a given osmolality because the blood volume deficit is sensed appropriately. Older adults respond to increased osmolality in a similar manner regardless of vascular volume. That is, thirst deficiency in the elderly occurs because of a reduced ability to sense a volume deficit; osmo-regulation is relatively intact. See also Figures 3 and 4.]
... response to repeated dehydrating stimuli also appears to be reduced, which may contribute to a relative inability to expand plasma volume. When age differences are noted in the physiological control systems associated with thirst and satiety, hypovolemia seems to be more closely associated with a decreased thirst sensation. Available evidence suggests that older men and women have a higher osmotic operating point for thirst sensation under normal daily conditions, and a diminished sensitivity to thirst and satiety reflexes arising from unloading (hypovolemia) and loading(hypervolemia) of baroreceptors, respectively.
Children
When exposed to high environmental heat, children are less effective thermoregulators* than adults because of their high surface area/mass ratio, underdeveloped sweating and skin blood flow mechanisms, and other factors (2).
[*Thermoregulation is the ability of an organism to keep its body temperature within certain boundaries, even when the surrounding temperature is very different. ]
Since thermoregulatory capacity in children is closely related to their hydration status, it is particularly important to understand alterations in the thirst mechanism of children that might lead to dehydration. Unfortunately, few studies have been performed that look at this issue from a mechanistic standpoint. Unlike the aging studies noted above, investigators have not examined separate and combined effects of stimulating thirst via hypovolemia and hypertonicity. This is a fruitful area for future research.
Voluntary dehydration in children. As is the case for young adults, children are susceptible to voluntary dehydration. Voluntary dehydration is defined as the lack of complete rehydration after a dehydrating stimulus because of inadequate or lack of prolonged thirst. In a study conducted by Bar-Or et al. (4), boys aged 10–12 yr exercised for 20–25 min, alternating with 20 min of rest, for a total of 3 hours in a hot environment. When allowed free access to 26°C water, the boys progressively dehydrated as the study continued. Mild voluntary dehydration occurs in well-acclimatized children living in tropical climates as well. Nine children (aged 13 ± 2 yr) were tested (28) under four conditions: sun exposure with forced drinking, sun exposure with voluntary drinking, shade with forced drinking, and shade with voluntary drinking. Forced drinking trials were those in which the amount of water (in a bottle at arm’s length at 15–17°C) consumed was the volume estimated to replace body weight losses. The subjects exercised for four 20-min sessions with 25 min of rest in between for a total of 180 min. Cumulative water intake was greater during the forced drinking trials compared with the ad libitum trials and cumulative weight loss was lower. Although thermoregulation was effective, a mild voluntary dehydration was noted. Voluntary water intake for the sun and shade conditions was 53% and 25% of their intake during the “forced”trials, respectively.Influence of drink flavoring on thirst and fluid intake. Palatability or taste of a beverage and drink composition have been shown to play a significant role in promoting fluid intake in adults. This is the case for children as well. Meyer and Bar-Or (16) had children aged 9 to 13 years exercise for 90 min in a hot, dry environment followed by a 30-min recovery, during which time drinks of varying flavors (grape, apple, orange, and water) were given ad *libitum. [*Ad lib: Abbreviation for the Latin "ad libitum" meaning "at pleasure" and "at one's pleasure, as much as one desires, to the full extent of one's wishes." Sometimes seen on a prescription or doctor's order.]
On the basis of visual analog scale ratings, the children’s thirst intensity began to increase after ~100 grams of body weight loss and increased with increasing dehydration. During recovery, however, most of the children voluntarily overhydrated with all the different flavored drinks. Grape and orange intake exceeded that for apple and water. Although grape was the preferred drink throughout the dehydration phase, its desirability did not increase as much as the desirability for orange, apple, and water with increasing dehydration. This indicates that during normally hydrated states, grape is the preferential flavor for children, but in times of dehydration, orange may be more greatly desired. It could be possible, however, that the grape-flavored drink reached a ceiling value for desirability. This study suggests that availability of flavored drinks after exercise-induced dehydration may promote increased fluid intake. However,it should be noted that the magnitude of dehydration in this study (like many pediatric studies) was small, about 290 g or 0.76% of body weight.
Influence of drink composition on thirst and fluid intake. Sweating rate is lower in children than in adults, as is the sodium concentration of the sweat. Therefore, total sodium losses in sweat tend to be lower in children, even when corrected for body mass (16). Inclusion of sodium in replacement drinks promotes drinking and may aid in fluid retention in the vascular space.
To examine the influence of sodium content on thirst and fluid intake in children, Meyer et al. (17,18) studied 9- to 12-yr-old children who were kept euhydrated* [*Normal state of body water content; absence of absolute or relative hydration or dehydration. ... euhydration the normal state of body water content (typically about 40 litres).] while cycling for three intermittent bouts followed by a high-intensity ride to exhaustion in 35°C. During a 30-min recovery period, the subjects were allowed to drink ad libitum one of four as-signed drinks that differed in sodium content. The drinks were sweetened grape-flavored water, grape-flavored 6% CHO with no sodium, grape-flavored 6% CHO with 8.8mEq·L⁻1 sodium, or grape-flavored 6% CHO with 18.5m Eq·L⁻1 sodium. There were no changes in plasma osmolality or sodium regardless of drink composition. Drink composition likewise did not affect drinking behavior during recovery, and volume intake was similar across trials(~200 mL). Perceived thirst and “stomach fullness” were similar across trials. Thus, well-hydrated children (with little thirst drive) show no preference for drinks on the basis of sodium concentration, even after exercise in a warm environment.
However, a follow-up study by the same group (37) again compared drinking responses to unflavored water, grape-flavored water, and grape-flavored water with 6% CHO and18.5 mEq·L⁻1 sodium. Boys aged 9 to 12 yr cycled at 35°C intermittently for a total of 180 min and drinks were available in a chilled bottle for ad libitum consumption without encouragement. Total drink intake by the end of sessions was 44.5% higher with flavored water than with water alone and 91% higher when flavoring, carbohydrate, and sodium were added to the water. In the CHO-Na beverage trials,
fluid intake exceeded fluid loss, whereas in the other two trials dehydration occurred (Fig. 7).
This study shows the importance of both flavor and composition in increasing fluid intake in children. This response is consistent across multiple days of exercise-heat exposure, as this CHO-N a beverage resulted in a positive fluid balance in 67 out of 72 sessions conducted over a 2-weeks period (38).
Finally, in a study conducted by Rivera-Brown et al. (27), twelve 11- to 14-year-old boys indigenous to a tropical climate cycled intermittently outdoors at a wet-bulb globe temperature of 30°C. These tropical natives had higher sweating rates than those measured in children in previous chamber trials. Each boy went through two exercise sessions: one with unflavored water and one with flavored 6% CHO and 18 mmol·L⫺1 Na solution (CHO-Na). They found that the subjects drank 32% more in the CHO-Na session than in the water-only session (Fig. 7). It was also noted that voluntary rehydration during the CHO-Na session resulted in a positive fluid balance, whereas the water resulted in a negative fluid balance (ineffective replacement). A preferred-flavor beverage containing 6% CHO and 18 mmol·L⁻1 Na promotes more drinking than water to help rehydrate children in exercising conditions similar to those of possible outdoor climates. In children, as in adults, it is clear that palatability and drink composition affect the volume of fluids voluntarily consumed during and after dehydrating exercise.
Osmotic thirst in children. Although no mechanistic studies have been performed on thirst stimulation in children, some clues can be gained from comparisons of healthy children with those with cystic fibrosis (CF). CF patients lose large amounts of NaCl in the sweat that would attenuate the increase in plasma osmolality. If plasma hypertonicity were a major drive for thirst, CF children would be expected to report lower thirst sensations and less fluid consumption.This has been demonstrated in a study by Bar-Or et al. (3),despite similar degrees of heat strain in CF patients and normal control children. In a subsequent study (13), addition of 30 mmol·L⫺1 NaCl did not increase voluntary drinking compared with water in such patients. However, when 50 mmol· L⫺1 NaCl was given, voluntary drinking increased and voluntary dehydration was prevented. This lends credence to the importance of osmotic thirst in children.
Conclusion. Children seldom voluntarily dehydrate in activities lasting 45 min or less (Bar-Or, O., personal communication). Flavoring drinks and adding NaCl in the range of ~18 mmol·L⫺1 increases ad libitum fluid intake. Few if any laboratory studies have been performed aimed at elucidating mechanistic differences of thirst in children, that is, examining differences when challenged by hyperosmotic versus hypovolemic stimuli. Data examining oropharyngeal metering in children are also lacking.
PRACTICAL IMPLICATIONS
Clearly, fluid replacement in children and the elderly should not rely on thirst alone. Education about proper hydration is an essential element for these two populations. In older adults, longer time periods should be given for rehydration after dehydration. In children, flavoring and NaCl content of the ingested fluids are important promoters of drinking. However, no specific changes in the composition of currently available carbohydrate-electrolyte drinks are recommended by the sparse data currently available. Neither age group is prone to chronic dehydration as previously suggested in the popular literature.
The authors are indebted to the Gatorade Sports Science Institute for their support of this review and wish to acknowledge the helpful editorial comments and suggestions of Drs. Oded Bar-Or,Gary Mack, Nina Stachenfeld, Bob Murray, and David Lamb.
Studies from the author’s laboratory were supported by National Institutes of Health grants R01-AG07004 and M01-RR10732.
Address for correspondence: W. Larry Kenney, Ph.D., FACSM,Noll Physiological Research Center, 102 Noll Laboratory, Penn State University, University Park, PA 16802; E-mail: w7k@psu.edu.FIGURE 7—Drinking response of boys aged 9–12 years during exercise. In children from both temperate and tropical climates, flavoring of water increased consumption over unflavored water. Adding 6% carbohydrate to the flavored water increased intake again compared with plain water. When flavored carbohydrate-electrolyte drinks are available, children rarely experience voluntary dehydration. (Redrawn from data published in Wilk and Bar-Or (37) and Rivera-Brown et al. (27).)AGE AND THIRST Medicine & Science in Sports & Exercise1531
REFERENCES
1. AGATE,J.The Practice of Geriatrics. London: Heinemann, 1970, p. 41.2.
2. BAR-OR, O. Temperature regulation during exercise in children and adolescents. In: C. G. Gisolfi and D. R. Lamb (Eds.). Perspectives in Exercise Science and Sports Medicine: Youth, Exercise, and Sport,Vol. 2. Carmel, IN: Benchmark Press, 1989, pp. 335–368.3.
3. BAR-OR, O., C. J. BLIMKIE, J.D.HAY, J.D.MACDOUGALL, D. S. WARD, and W. M. WILSON. Voluntary dehydration and heat intolerance in cystic fibrosis. Lancet 339:696–699, 1992.4.
4. BAR-OR, O., O. INBAR, A.ROTHSHTEIN, and H. ZONDER. Voluntary hypohydration in 10- to 12-year-old boys. J. Appl. Physiol. 48:104–108, 1980.5.
5. CROWE, M. J., M. L. FORSLING, B.J.ROLLS, P.A.PHILLIPS, J.G.G.LEDINGHAM, and R. F. SMITH. Altered water excretion in healthy elderly men. Age Ageing 16:285–293, 1987.6.
6. DE CASTRO, J. M. A micro regulatory analysis of spontaneous fluid intake by humans: evidence that the amount of fluid ingestion and its timing is governed by feeding. Physiol. Behav. 43:705–714,1988.7.
7. DE CASTRO, J. M. The relationship of spontaneous macro nutrient and sodium intake with fluid ingestion and thirst in humans. Physiol. Behav. 49:513–519, 1991.8.
8. DE CASTRO, J. M. Age-related changes in natural spontaneous fluid ingestion and thirst in humans. J. Gerontol. 47:P321–P330, 1992.9.
9. FAULL, C. M., C. HOLMES, and P. H. BAYLIS. Water balance in elderly people: is there a deficiency of vasopressin? Age Ageing 22:114–120, 1993.10.
10. FIGARO, M. K., and G. W. MACK. Control of fluid intake in dehydrated humans: role of oropharyngeal stimulation. Am.J. Physiol. 272:R1740–R1746, 1997.11.
11. GISOLFI, C. V., R. W. SUMMERS,H.P.SCHEDL, and T. L. BLEILER. Intestinal water absorption from select carbohydrate solutions in humans. J. Appl. Physiol. 73:2142–2150, 1992.12.
12. KENNEY, W. L., C. G. TANKERSLEY, D.L.NEWSWANGER, D.E.HYDE, and S. M. PUHL. Age and hypohydration independently influence the peripheral vascular response to heat stress. J. Appl.Physiol. 68:1902–1908, 1990.
13. KRIEMER, S., B. WILK,W.SCHURER,W.M.WILSON, and O.BAR-OR. Preventing dehydration in children with cystic fibrosis who exercise in the heat. Med. Sci. Sports Exerc. 31:774–779, 1999.
14.Lo¨WIK,M.R.H.,S.WESTENBRINK,K.F.A.M.HULSHOF,C.KISTE-MAKER, and R. J. J. HERMUS. Nutrition and aging: dietary intake ofapparently healthy elderly. J. Am. Coll. Nutr. 8:347–356, 1989.
15. MACK, G. W., C. A. WESEMAN, G.W.LANGHANS, H.SCHERZER,C. M. GILLEN, and E. R. NADEL. Body fluid balance in dehydrated healthy older men: thirst and renal osmoregulation. J. Appl.Physiol. 76:1615–1623, 1994.
16. MEYER, F., and O. BAR-OR. Fluid and electrolyte loss during exercise: the paediatric angle. Sports Med. 18:4–9, 1994.
17. MEYER, F., O. BAR-OR,D.MACDOUGALL, and G. J. F. HEIGEN-HAUSER. Drink composition and the electrolyte balance of children exercising in the heat. Med. Sci. Sports Exerc. 27:882–887, 1995.
18. MEYER, F., O. BAR-OR,A.SALSBERG, and D. PASSE. Hypohydration during exercise in children: effect on thirst, drink preferences, and rehydration. Int. J. Sports Med. 4:22–35, 1994.
19. MIESCHER, E., and S. M. FORTNEY. Responses to dehydration and rehydration during heat exposure in young and older men. Am.J. Physiol. 257:R1050–R1056, 1989.
20. O’NEILL, P. A., E. B. FARAGHER, I.DAVIES,R.WEARS, K.A.MCLEAN, and D. S. FAIRWEATHER. Reduced survival with increasing plasma osmolality in elderly continuing care patients. Age Ageing 19:68–71, 1990.
21. PHILLIPS, P. A., M. BRETHERTON, C.I.JOHNSTON, and L. GRAY. Reduced osmotic thirst in healthy elderly men. Am. J. Physiol.261:R166–R171, 1991.
22. PHILLIPS, P. A., M. BRETHERTON, J.RISVANIS, D.CASLEY, C.JOHNSTON, and L. GRAY. Effects of drinking on thirst and vasopressin in dehydrated elderly men. Am. J. Physiol. 264:R877–R881, 1993.
23. PHILLIPS, P. A., C. I. JOHNSTON, and L. GRAY. Thirst and fluid intake in the elderly. In: D. J. Ramsay and D. A. Booth (Eds.). Thirst:Physiological and Psychological Aspects. London: Springer-Ver-lag, 1991, pp. 403–411.
24. PHILLIPS, P. A., and B. J. ROLLS. Thirst and dehydration. In: M.Fiatarone-Singh (Ed.). Exercise, Nutrition and the Older Woman:Wellness for Women Over 50. Boca Raton, FL: CRC Press, 2000,pp. 443–452.
25. PHILLIPS, P. A., B. J. ROLLS,J.G.G.LEDINGHAM, and J. J. MORTON.Body fluid changes, thirst and drinking in man during free access to water. Physiol. Behav. 33:357–363, 1984.
26. PHILLIPS, P. A., B. J. ROLLS, M.L.LEDINGHAM, et al. Reduced thirst after water deprivation in healthy elderly men. N. Engl. J. Med.311:753–759, 1984.
27. RIVERA-BROWN, A. M., R. GUTIERREZ, J.C.GUTIERREZ, W.R.FRONTERA, and O. BAR-OR. Drink composition, voluntary drinking,and fluid balance in exercising, trained, heat-acclimatized boys. J. Appl. Physiol. 86:78–84, 1999.
28. RODRIGUEZ-SANTANA, J. R., A. M. RIVERA-BROWN, W.R.FRONTERA, M. A. RIVERA, P.M.MAYOL, and O. BAR-OR. Effect of drink pattern and solar radiation on thermoregulation and fluid balance during exercise in chronically heat acclimatized children. Am.J. Hum. Biol. 7:643–650, 1995.
29. ROLLS, B. J. Homeostatic and non-homeostatic controls of drinking in humans. In: M. J. Arnaud (Ed.). Hydration Throughout Life.
Montrouge, France: John Libbey Eurotext, 1998, pp. 19–28.
30. SCHOORLEMMER, G. H. M., A. K. JOHNSON, and R. L. THUNHORST. Effect of hyperosmotic solutions on salt excretion and thirst in rats. Am. J. Physiol. 278:R917–R923, 2000.
31. SNYDER, M. A., D. W. FEIGAL, and A. L. ARIEFF. Hypernatraemia* in elderly patients: a heterogenous, morbid and iatrogenic^^ entity. Ann. Intern. Med. 107:309–319, 1987.[*Hypernatremia is a common electrolyte problem that is defined as a rise in serum sodium concentration to a value exceeding 145 mmol/L. [1, 2, 3] It is strictly defined as a hyperosmolar condition caused by a decrease in total body water (TBW) relative to electrolyte content. ] [^^iatrogenic,ʌɪˌatrə(ʊ)ˈdʒɛnɪk/adjective/relating to illness caused by medical examination or treatment."drugs may cause side effects which can lead to iatrogenic disease" ]
32. SPANGLER, P. F., T. R. RISLEY, and D. D. BILYEW. The management of dehydration and incontinence in non-ambulatory geriatric patients. J. Appl. Behav. Anal. 17:397–401, 1984.
33. STACHENFELD, N. S., L. DIPIETRO,E.R.NADEL, and G. W. MACK. Mechanism of attenuated thirst in aging: role of central volume* receptors. Am. J. Physiol. 272:R148–R157, 1997.
[*Atrial volume receptors are low pressure baroreceptors that are found in the atria of the heart and carotid arteries.
When these receptors detect a blood volume decrease in the atria, a signal is transmitted from the receptors to the hypothalamus in the brain. The hypothalamus, in turn, increases the production of vasopressin (ADH, AVP, or arginine vasopressin). These receptors also cause a renal vasodilation, resulting in increase of the water amount in the glomerular filtrate which, combined with the increased production of vasopressin by the hypothalamus, will cause water retention in urine. This increases the blood volume, resulting in the increase of blood pressure.]





Am. J. Physiol. 272:R148–R157, 1997.
34. STACHENFELD, N. S., G. W. MACK,A.TAKAMATA,L.DIPIETRO, and E. R. NADEL. Thirst and fluid regulatory responses to hypertonicity in older adults. Am. J. Physiol. 271:R757–R765, 1996.
35. STRICKER, E. M., and J. G. VERBALIS. Hormones and behavior: the biology of thirst and sodium appetite. Am. Sci. 76:261–267, 1988.
36. TAKAMATA, A., T. ITO,Y.KAZUHIRO, et al. Effect of an exercise-heat acclimation program on body fluid regulatory responses to dehydration in older men. Am. J. Physiol. 277:R1041–R1050,1999.
37. WILK, B., and O. BAR-OR. Effect of drink flavor and NaCl on voluntary drinking and hydration in boys exercising in the heat.
J. Appl. Physiol. 80:1112–1117, 1996.
38. WILK, B., S. KRIEMLER,H.KELLER, and O. BAR-OR. Consistency in preventing voluntary dehydration in boys who drink a flavored carbohydrate-NaCl beverage during exercise in the heat.
Int.J. Sports Nutr. 8:1–9, 1998.
39. ZAPPE, D. H., G. W. BELL, H.SWARTZENTRUBER, R.F.WIDEMAN, and W. L. KENNEY. Age and regulation of fluid and electrolyte balance during repeated exercise sessions. Am. J. Physiol. 270:R71–R79, 1996
Influence of Age on Thirst and Fluid Intake (PDF Download Available). Available from: https://www.researchgate.net/publication/11818351_Influence_of_Age_on_Thirst_and_Fluid_Intake [accessed Jun 3, 2017].


turgor; təːɡə, the state of turgidity and resulting rigidity of cells or tissues, typically due to the absorption of fluid. "turgor pressure".
If no dehydration is present, the skin returns quickly to the normal position. With moderate to severe dehydration, decreased skin turgor causes the pinched-up .
W. LARRY KENNEY and PERCY CHIU
Noll Physiological Research Center and Schreyer Honors College, Penn State University, University Park, PA 16802
ABSTRACT
KENNEY, W. L., and P. CHIU.
Influence of age on thirst and fluid intake.
Med. Sci. Sports Exerc., Vol. 33, No. 9, 2001, pp.1524–1532. Independently living older adults (over the age of 65 yr) consume adequate volumes of fluids on a daily basis. However,when challenged by fluid deprivation, a hyperosmotic stimulus, or exercise in a warm environment (all of which combine hypovolemia and hyperosmolality), older adults exhibit decreased thirst sensation and reduced fluid intake. Full fluid restoration eventually occurs, but full restoration of fluid balance is slowed. The aging process alters important physiological control systems associated with thirst and satiety. Recent evidence suggests that older men and women (i) have a higher baseline osmolality and thus a higher osmotic operating point for thirst sensation (with little or no change in sensitivity), and (ii) exhibit diminished thirst and satiety in response to the unloading (hypovolemia) and loading (hypervolemia) of baroreceptors. A diminished sensation of thirst in the elderly relative to young adults is generally absent when a volume stimulus is absent, despite higher baseline plasma osmolalities. Compared with the elderly, there are scant data associated with homeostatic control of thirst in children. Non homeostatic control of thirst and drinking behavior may likewise be different for children (as it is for the elderly), as compared with young adults; however, little empirical data exist on this topic. Children rarely exhibit voluntary dehydration for activities lasting 45 min or less; however, drink flavoring and sodium chloride are important promoters of drinking in active children.
Key Words: AGING, DRINKING BEHAVIOR, CHILDREN,ELDERLY, OSMOLALITY, BLOOD VOLUME, HYDRATION, DEHYDRATION.
[Osmolality of blood increases with dehydration and decreases with over hydration. In normal people, increased osmolality in the blood will stimulate secretion of antidiuretic hormone (ADH). This will result in increased water reabsorption, more concentrated urine, and less concentrated blood plasma.] [Read about "Plasma osmolality" click here]
The health benefits of proper hydration have long been recognized, both regular daily hydration (unchallenged) and in response to dehydration (the process by which an acute fluid deficit occurs) or hypo-hydration (the term that connotes the level of fluid deficit). A major component of this rehydration process involves thirst which—depending on drink availability—leads to voluntary fluid intake. The manifestations of thirst have been characterized as a combination of sensations that increase with dehydration and decrease with rehydration (restoration of fluid balance), including a dry, scratchy mouth and throat,chapped and dry lips, light-headedness, dizziness, tiredness,irritability, headache, loss of appetite, and feeling of an“empty stomach” (24).
FIGURE 1—Homeostatic versus nonhomeostatic control of thirst in humans. Under stressed (dehydrated) conditions, thirst results from increases in cellular tonicity and decreases in extracellular volume. Nonhomeostatic controls include a variety of influences, including—but not limited to—those shown here.
FIGURE 1—Homeostatic versus nonhomeostatic control of thirst in humans. Under stressed (dehydrated) conditions, thirst results from increases in cellular tonicity and decreases in extracellular volume. Nonhomeostatic controls include a variety of influences, including— but not limited to—those shown here.
Thirst results from a complex interaction of physiological control systems and behavioral influences. Figure 1 shows the distinction between physiologically determined thirst and drinking behavior that is under the influence of non homeostatic control. Physiological thirst results from dehydration (no further distinction will be made here between dehydration and hypo-hydration) and is stimulated by two main homeostatic mechanisms: increases in cellular tonicity (cellular dehydration) and decreases in extracellular fluid volume (extracellular dehydration). The former is sensed by osmoreceptors in the central nervous system, whereas the latter is monitored by baroreceptors in the vascular compartment. Since dehydration causes fluid losses from the intracellular and extracellular spaces, redundant sensing for the purposes of fluid balance decreases the likelihood of error in these feedback loops.
Cellular dehydration is an important thirst stimulus in humans. Drinking is stimulated by increases in the effective osmotic pressure of the plasma. Central (and possibly peripheral) osmoreceptors sense the level of dehydration and feed back to the hypothalamus to maintain homeostasis. In animal models, thirst depends on a tonicity sensor that is located outside the blood-brain barrier, possibly in one of the circumventricular* organs of the brain (30).[*Circumventricular organs (CVOs) are structures in the brain that are characterized by their extensive vasculature and lack of a normal blood brain barrier (BBB). ] Localization of primary osmosensing organ(s) is lacking in humans, but it is likely also located in this region. Depending on these osmoreceptors, thirst thresholds are set and thirst is stimulated on the basis presumably of an error signal (i.e., the deviation of the sensed plasma osmolality from some “normal” operating point). This system has been modeled as a single feedback loop (35) as depicted in the left portion of Figure 2.
Extracellular dehydration as a thirst stimulus is more complex, as depicted on the right-hand side of Figure 2. This double feedback loop involves both baroreceptors in large vessels, which are activated with decreases in blood volume,and renal mechanisms, which elicit the renin-angiotensin-aldosterone system in response to decreased renal perfusion and other stimuli. Hormonal activation of a salt appetite(more well defined in animal models than in humans) adds to the complexity of both volume and osmo regulation of thirst (Fig. 2). This mechanism, however, has been suggested to be the less predominant of the two in young adults,and it has been suggested that decreased extracellular volume becomes a fundamental thirst stimulus only in cases of severe dehydration (29). However, as discussed later in this article, strong data to the contrary exist (e.g., Stachenfeld etal. (33)). The relative influences of intra- and extracellular dehydration in children is undetermined. In the elderly, a clearer picture is beginning to emerge with respect to these mechanisms. In general, although regulation of the physio-logical thirst mechanism has long been studied in young adults, many important questions remain with respect to differences in thirst sensation and fluid intake in children and the elderly.
A third mechanism that helps regulate thirst also deserves mention. In humans, the act of swallowing helps to regulate the volume of fluid ingested by providing an integrated signal proportional to the cumulative ingested volume(termed “oropharyngeal metering”). Figaro and Mack (10)dehydrated six subjects by light exercise in a warm environment on three different occasions (⫺28.6 mL·kg power to minus1 body-weight (BW)). Rehydration involved one of three treatments(all occurring with a nasogastric (NG) feeding tube insert-ed). The first involved 75 min of ad libitum drinking (which averaged 20.0 plus-minus 2.0 mL·kg (power to the minus 1) BW). The second rehydration treatment involved the infusion of an identical volume directly into the stomach via the NG tube plus ad libitum drinking after 25 min. The third treatment involved ad libitum drinking again, but with immediate withdrawal of the fluid from the stomach. Reflex inhibition of thirst began within 5 min of rehydration in groups 1 and 3, but not in the infusion group. Ad libitum drinking without absorption(withdrawn with NG tube) resulted in only 15% more fluid intake than the ad libitum condition. These data demonstrate a clear role of esophageal metering in determining fluid intake during dipsogenic stimuli in humans.
In addition to the homeostatic mechanisms mentioned above, there are also myriad non homeostatic controls that add to the stimulation of thirst. These include a wide array of psychological and environmental influences such as availability of the beverage; taste, temperature, and palatability of the beverage; knowledge about the importance of proper hydration; drinking in association with meals; social and societal norms and habits; and even the presence of others who are consuming a beverage. Ad libitum drinking is typically done in association with meals. When a variety of foods and drinks are available, spontaneous drinking occurs and exceeds the volume necessary for fluid balance(29), with excess fluid eliminated by the kidneys. This is true not only for young adults but also for children and for healthy independently living older adults (8). Given free access to fluid, humans become thirsty and drink before body fluid deficits appear, perhaps in response to subtle oropharyngeal cues or simply because of habit or social norm (29). Undoubtedly, such behavioral cues are different in children and in the elderly, but little research has been performed in this important area.
EXPERIMENTAL THIRST STIMULATION
Most laboratory and field studies of thirst have invoked a dehydrating stimulus such as restricted access to fluid in-take, prolonged dynamic exercise (often performed in a warm environment), or infusion of hypertonic saline. Such studies then allow unrestricted access to monitored fluids during a rehydration period after dehydration, or the subjects are allowed unrestricted access to monitored fluids throughout a multi day trial. Table 1 lists several types of the various perturbations that have been used in published studies on older adults. Fluid deprivation and exercise both create a hypovolemic, hyperosmotic condition, the most common milieu associated with dehydration. Hypertonic saline infusion can provide either a relatively euvolemic or hypervolemic hyperosmotic condition, depending on the volume and tonicity of the infusate. And finally, drives for thirst and for satiety can be provided simultaneously in the laboratory, for example, by head-out water immersion ...
[FIGURE 1—Homeostatic versus non homeostatic control of thirst in humans. Under stressed (dehydrated) conditions, thirst results from increases in cellular tonicity and decreases in extracellular volume. Non homeostatic controls include a variety of influences, including—but not limited to—those shown here.]
[FIGURE 2—Simplified model for homeostatic control of thirst showing feedback loops and redundancy (redrawn from Stricker and Verbalis (35)). Osmoregulatory thirst is a single feedback loop with correction proceeding until the dehydration is corrected. Hypovolemic thirst is modeled as a double-loop negative feedback system in which water alone cannot correct the plasma volume deficit. Therefore, water intake is not maintained despite the presence of a hypovolemic stimulus. Sodium intake serves to expand plasma volume and to avoid excess osmotic dilution.]
... immediately following dehydration (33). Although such experiments have yielded important data for older adults, no such data exist for children.
TABLE 1. Summarized studies of various laboratory methods of thirst stimulation in older adults according to the stimulus used to evoke thirst.
Perturbation ↑O ↓V Effect on Thirst (Relative to Young Subjects), Study (Reference)
1.Fluid restriction ↑ ↓ Decreased thirst and fluid intake for a given weight loss, Phillips and Roll (25)
2.Exercise in the heat ↑ ↓ Decreased thirst ratings; fluid intake matched thirst ratings; osmolality threshold elevated and sensitivity reduced, Mack et al. (15)
3.Passive prolonged heat stress ↑ ↓ Decreased thirst ratings but similar fluid intakes, Miescher and Fortney (19)
4.Hypertonic saline infusion ↑ ( Decreased thirst ratings, Phillips et al. (21)
5.Hypertonic saline infusion ↑ (↓) Similar thirst ratings; similar plasma arginine response, Stachenfeld et al. (34)
6.Exercise in the heat; head-out immersion ↑ (↓) Decreased thirst before immersion; restoration of central volume reduced thirst and drinking only in young subjects, Stachenfeld et al. (33)
7.Thirst suppression by fluid loading (↓) (↑) Thirst blunted in young subjects only, Crowe et al. (5) and Phillipset al. (22)
8.Exercise-heat acclimation ↑ ↓ Decreased fluid intake in older subjects during recovery from daily exercise (6 d) led to inability to expand plasma volume, Takamata et al. (36)
9.Exercise-heat acclimation ↑ ↓ Decreased daily fluid intake in older subjects over a 4-d exercise period led to inability to expand plasma volume, Zappe et al. (39)
Body weight before and after experiments, plasma volume, and plasma osmolality measurements are typically the dependent variables used to assess rehydration efficacy.However, visual analog scales of thirst ratings and questionnaires are still the standard methods used to quantify thirst. Reliable and valid use of subjective scales may be problematic for children and some elderly subjects. Further-more, several discrepancies appear in the literature with respect to thirst ratings under “baseline euhydrated” conditions (e.g., Mack et al. (15)).
RESEARCH REVIEW
Older Adults
The gerontology literature contains multiple reports of altered hydration status in the elderly. Careful reading suggests that most of this information comes from anecdotal evidence and facts extrapolated from clinical and institutionalized older populations. For example, in one study,dehydration was evident in about 25% of non ambulatory geriatric hospital patients (32). Another article reported that a majority of patients over age 65 from six continuing care hospital wards had elevated serum osmolalities (>296mOsm·kg to the power minus1), and a group of 58 patients randomly selected had a mean plasma osmolality of 304 plus-minus 8 mOsm·kg to the power minus1 at time of hospital admission (20). As further evidence of a problem with hydration in the elderly, a common textbook observation is that when older patients are hospitalized,many cannot or will not spontaneously ask for fluids (1).Extrapolating such statistics to non institutionalized, healthy older men and women leads to the inaccurate conclusion that many older individuals walk around in a frank state of hyperosmolar hypo-hydration. This does not appear to be the case.
Despite the statistics cited above for geriatric hospitals,dehydration is evident in only about 1% of older patients admitted to community hospitals, a better indicator of the health status of independently living adults (31). Even in the hyperosmolar institutionalized patients surveyed by O’Neillet al. (20) (ages 67–101 yr), there was no correlation be-tween age and osmolality. Therefore, it is more plausible that dehydration in the elderly (i) accompanies, or results from, various clinical conditions and/or medications, or (ii)reflects an age-specific response to mild water deprivation(discussed in detail below). Both the incidence and the magnitude of chronic dehydration in the healthy community-dwelling older adult are overstated. However, to err on the side of safety, proper hydration practices during high-risk times (e.g., projected heat waves, long duration activity in hot environments) should be taught and fluid intake should be emphasized in this population.Spontaneous fluid ingestion by healthy older adults. Do older men and women, on a day-to-day basis,consume less fluid than younger men and women? What dictates spontaneous ad libitum fluid intake, and do those stimuli change as we age? Under ad libitum conditions, in natural environments, neither the amount nor the pattern of fluid intake is regulated physiologically to any great extent(6,25). Rather, both are governed by the amount and timing of food intake (6,7,25). Enough fluid is consumed with meals to maintain adequate fluid balance, and under unstressed conditions the renal response is sufficient to maintain this balance.
This concept seems to apply to the older adult population as well. When fluids are readily available, independently living healthy older individuals have daily fluid intakes that are similar to those of younger individuals. In one study, 262 adults aged 20–80 yr were asked to maintain a food and fluid intake diary for 7 consecutive days. There were no notable age differences in total fluid intake (food water content plus fluids drunk), water intake in excess of that required for digestion (“surplus water”), or overall volume of fluid consumed. Nor was there an age effect for thirst, its relationship to fluid intake, or the amount of fluid ingested relative to the amount of solids ingested during a meal (8).Even in those few surveys of community-dwelling older men and women that report slight reductions of fluid intake,their intake is not substantially reduced. In a Dutch survey of 539 healthy, independently living adults aged 65–79 yr,daily water intake averaged 2.15 L·d⫺1for men and 1.98L·d⫺1for women. Although the nonalcoholic beverage in-take of the 75- to 79-yr-old group was lower than that of younger subjects, even the lowest daily intake reported(1.87 L·d⫺1) was well within what the authors considered the normal range of 1.6–2.4 L·d⫺1(14). However, it is important to realize, as pointed out by Rolls (29), that if older individuals do not feel well or if access to palatable fluids is in any way restricted, problems may develop.
Thus, enough fluid is consumed in response to non regulatory stimuli (i.e., with meals) to maintain adequate fluid balance, and under unstressful conditions the kidney response of older persons is sufficient to maintain this balance. Therefore, afferent physiological signals that arise from a fluid deficit are rarely produced, and physiologically mediated mechanisms are seldom called on under conditions of normal daily life (8). This may be especially true for the older adult population, which as a population tends toward a more sedentary lifestyle.
“Baseline” osmolality, plasma volume, and euhydration in the elderly. On the surface, it seems difficult to reconcile the above discussion with data from several laboratory studies. When older subjects report for laboratory studies designed to challenge fluid balance, they are typically in a normal state of hydration (5,12,35), but an elevated plasma osmolality (typically by about 3– 6m Osm·kg to the power minus1) is often noted in these older subject groups at“baseline” (5,9,15,19). Such small differences in blood tonicity have led to the conclusion that “healthy, active older[individuals] are hyperosmotic and hypovolemic” (15).However, such studies typically require an overnight fast without pre experimental fluid intake; thus, the “baseline”plasma variables that are reported in some studies may actually reflect a dehydrated state. An overnight fast should more accurately be viewed as a mild dehydration, which may selectively render older subjects slightly hyperosmotic and hypovolemic if renal function is altered. This is clearly not the entire reason for elevated plasma osmolalities in older subjects, since differences are seen even in studies where pre-exercise fluid intake is standardized (15). Further-more, when older and younger subjects are matched for maximal aerobic capacity and body composition, baseline differences in both plasma osmolality and plasma volumeare minimized (12). Because the elevated osmolality of older men and women is not associated with elevated plasma sodium concentrations, it may better reflect elevations in substances like glucose and blood urea nitrogen.
Dehydration and aging: non thirst factors. Voluntary fluid intake after dehydration is clearly influenced by non thirst factors such as the availability of fluids and their palatability. Although thirst and volume of fluid ingested are separate entities, they seem to be affected in parallel by age,and increasing the availability or palatability of fluids does not seem to significantly increase water deprivation-induced fluid intake in older men and women (23). After two separate bouts of dehydration (fluid deprivation plus a dry diet),healthy older men were offered either water, mineral water,or a variety of other palatable beverages, including cola and orange juice (23). Orange juice was consumed in larger volumes on single occasions, suggesting a higher palatability, yet over a 2-h period there was no difference in fluid consumption between trials or beverages. Although these results imply that palatability alone is insufficient to over-come the reduced thirst sensation associated with aging, the tonicity of the fluid consumed may be important in the time course of drinking (11) and in the effectiveness of re-hydration (22).
Aging and thirst. Under normal conditions of daily living, increased thirst and fluid intake defend against any threats to fluid homeostasis that may result from altered free-water clearance by the kidneys. Therefore, although an inadequate renal response to mild water deprivation may play a role in any fluid volume depletion occurring in older persons, reduced thirst is probably more important (22). Ad libitum fluid intake can be directly measured, but thirst is typically assessed using visual analog scales involving questions such as, “How thirsty do you feel now?” Care should be taken to ensure that older subjects interpret such scales and rate their thirst sensations in a manner similar to younger subjects.
As shown in Figures 1 and 2, thirst can be elicited by situations or manipulations that decrease extracellular fluid volume, increase intracellular tonicity, or both. Most natural situations, such as exercise, exogenous heat stress, and fluid deprivation, simultaneously decrease volume and increase tonicity. After a 24-h period of restricted water intake that caused an equal weight loss in older and younger subjects,a group of healthy men 67–75 yr old were less thirsty and replaced less of the fluid deficit over the next 2 h than did young controls (26). This initial finding of reduced thirst with advancing age has been confirmed using exercise/heatstress to induce both a volume deficit and hyperosmolality(15). Additionally, Mack et al. (15) showed that the relationship between thirst rating and fluid intake was not altered by age. Conversely, data from Miescher and Fortney(19) dissociated thirst ratings from fluid intake in older men after a prolonged passive heat stress; that is, the older men were thirstier but drank the same volume of water. When both volume and tonicity are affected by dehydration, older individuals operate around a higher plasma osmolality (a shift in the operating point of the system) and on a less steep portion of the stimulus-response curve (15).
Volume or osmolality deficit? Since either hypovolemia or hypertonicity can independently cause sensations of thirst, a compelling question is whether one of these control loops (depicted in Fig. 2) is significantly altered by the aging process, or whether both are impaired. Table 1 presents a variety of studies that independently or simultaneously decreased intravascular volume or increased plasma osmolality. Infusion of hypertonic saline has been used to increase osmolality (and create an osmotic thirst drive)while increasing plasma volume (i.e., creating a hyperosmolar hypervolemia). Phillips et al. (21) infused hypertonic saline (0.855 M) over a 2-h period in older and younger men. Although both age groups experienced an increased thirst sensation and water intake, the older men reported feeling less thirsty and drank less room-temperature water.Alternately, when Stachenfeld et al. (34) performed a similar study, osmotically stimulated increases in thirst were unaffected by age. Three methodological differences should be noted between these two studies. In the study by Phillipset al., subjects appeared at the laboratory after an overnight
fast, whereas the subjects in the study by Stachenfeld et al. ate a light breakfast and drank ~5 mL·kg⫺1 of water 1 hour before the experiment. Neither study reported a baseline difference in plasma osmolality between age groups. Second, Stachenfeld and colleagues infused 40% more saline(although the sodium load was similar), raising PV by 16–18% in both age groups. Phillips caused a significant PV expansion (by 9%) in the young men only. Finally, and perhaps most importantly, subjects were tested supine by Phillips et al. and upright by Stachenfeld et al. Therefore, in the former, baroreceptors were unloaded before the saline infusion.
FIGURE 3—Data are shown from three published studies (15,36,34) in which thirst ratings (standardized here as percentage of the full visual analog scale used to rate thirst subjectively) were plotted against plasma osmolality. Solid arrows connect predehydration and postdehydration data for young subjects in each panel; dashed arrows connect data points for older subjects. Baseline data points in each age group and experiment are circled. Panels a and b involved thermal dehydration, and baseline age differences were present for plasma volume and plasma osmolality. When there was no age difference in plasma volume (panel c; hypertonic saline infusion) and volume was expanded in both age groups, osmolar regulation of thirst was not different between young and older men. The authors speculated that plasma volume expansion modulated thirst in young, but not in older, subjects. See Figure 5 also.
Age and thirst suppression. The inverse of causing thirst by fluid deprivation is blunting thirst by oral fluid loading or expansion of (or a central shift in) blood volume. Crowe et al. (5) found that after young adults ingested 20mL·kg to the power of minus 1 water loads, thirst was suppressed for 1–2 hours and then increased progressively over the following 5–6 hours,whether they were initially fluid-depleted or not. Conversely, water-replete older men (mean age, 72 yr) showed no alteration in their thirst ratings over the entire 7 h after the water loads, despite clear indications that an osmotic thirst stimulus had occurred. Phillips et al. (22) also studied water-deprived (24 h) older and young men. Although thirst increased after water deprivation in both groups, it increased less in the elderly. When oral water loads of 10 mL·kg⫺1were subsequently given over a 2- to 3-min period, thirst was suppressed in both age groups; however, plasma AVP fell immediately after drinking only in the young group.These results demonstrate reduced oropharyngeal inhibition of AVP secretion in healthy older men despite maintained inhibition of thirst.
More recently, Stachenfeld et al. (33) used a novel experimental design to test the influence of central blood volume on thirst. After older and younger adults dehydrated by overnight water restriction and subsequent exercise in the heat, they recovered with or without head-out immersion(HOI). HOI forces blood volume centrally, loading baroreceptors and mimicking hypervolemia (or in this case, minimizing hypovolemia). In the young subjects, HOI caused an immediate fall in thirst perception and a dramatic reduction in ad libitum fluid intake (Fig. 4).
FIGURE 4 —When older (70 2 yr) and young (24 1 yr) subjects undergo dehydration, the sensation of thirst increases to a greater extent in the young subjects. When central fluid volume is restored acutely by head-out immersion, thirst is attenuated in young subjects only, even though 70% of the plasma volume loss was restored in the older men. This suggests that age differences in thirst arise from changes in the cardiovascular system (i.e., baroreceptor function or responsiveness). In both age groups, fluid intake followed thirst ratings . (Data redrawn from Stachenfeld et al. (33).)
A similar central blood volume expansion had no effect on thirst in the older subjects, however. Figure 5 presents a model for the foregoing discussion and conclusion.
It appears that when the sole stimulus for thirst and drinking is osmotic, there is little difference in thirst sensation in older adults compared with their younger counterparts. A deficit in the sensitivity of volume receptors appears to be a more important mechanism accounting for reduced thirst with aging.
Thirst during repeated exposures (acclimation). Body fluid regulation is influenced by acclimation status. In young adults, repeated bouts of exercise in hot environments results in an expansion of plasma volume primarily because of increased voluntary fluid intake (39). Zappe and colleagues (39) exercised young and older (67 plus-minus 1 yr old) adults in a 30°C environment for 4 consecutive days while monitoring PV, renal function, and daily 24-h fluid intake(Fig. 6c–e). Whereas the young subjects increased PV by10%, the older men did not expand their plasma volume significantly. This failure to increase intravascular volume was not caused by impaired renal water conservation but ...
[ FIGURE 3—Data are shown from three published studies (15,36,34) in which thirst ratings (standardized here as percentage of the full visual analog scale used to rate thirst subjectively) were plotted against plasma osmolality. Solid arrows connect pre-dehydration and post-dehydration data for young subjects in each panel; dashed arrows connect data points for older subjects. Baseline data points in each age group and experiment are circled.Panels a and b involved thermal dehydration, and baseline age differences were present for plasma volume and plasma osmolality. When there was no age difference in plasma volume (panel c; hypertonic saline infusion) and volume was expanded in both age groups, osmolar regulation of thirst was not different between young and older men. The authors speculated that plasma volume expansion modulated thirst in young, but not in older, subjects. See Figure 5 also.]
... rather by a smaller increase in 24-h fluid intake, which averaged 32 mL·kg to the power minus1·d to the power minus1in the older men versus 45mL·kg to the power minus1·d to the power minus1 in the younger men. These findings were later confirmed during a 6-d heat acclimation protocol (36) (Fig.6a and b).
After daily low-intensity intermittent exercise for 6 d,young men expanded PV by 5%, whereas the older men did not. During a 2-h recovery period after each exercise session, young men replaced, on average, 80% of lost fluid drinking a carbohydrate-electrolyte drink, compared with 34% fractional fluid recovery in the 70-yr-old group. This greater involuntary dehydration was accompanied by reduced thirst ratings, lower plasma vasopressin and aldosterone concentrations, and less renin activity. The plasma osmolality-thirst relationship was shifted rightward in the older subjects, i.e., a higher baseline plasma osmolality and elevated osmolar thirst threshold (pre-acclimation data are shown in Fig. 3b). However, the acclimation protocol had little effect on osmo-regulation of thirst, leading the authors to implicate attenuated baroreflex* (volume) control.
[*The baroreflex provides a rapid negative feedback loop in which an elevated blood pressure reflexively causes the heart rate to decrease and also causes blood pressure to decrease. Decreased blood pressure decreases baroreflex activation and causes heart rate to increase and to restore blood pressure levels. ]
They speculated that the older men may have had a lower baroreflex sensitivity and the acclimation program did not further attenuate this sensitivity, thus fluid intake was not altered.
Conclusion. When challenged by fluid deprivation, a hyperosmotic stimulus, hypovolemia, or exercise in a warm environment, older adults exhibit a decreased thirst sensation and reduced fluid intake. Acutely, fluid restoration is eventually effective, but restoration of fluid balance is slower. Longer term fluid intake (i.e., days to weeks) in
[FIGURE 6—A critical component of heat acclimation is the expansion of plasma volume during the first 2–5 days.
FIGURE 6 —A critical component of heat acclimation is the expansion of plasma volume during the first 2–5 d. This involves increased fluid intake and increased plasma protein translocation. Data from Takamata et al. (36) (panels a and b) and Zappe et al. (39) (panels c– e) show that plasma volume expansion is attenuated in older subjects, as is postexercise fluid intake and daily fluid intake during the initial acclimation stage.
[ FIGURE 4—When older (70 2 yr) and young (24 ⴞ 1 yr) subjects undergo dehydration, the sensation of thirst increases to a greater extent in the young subjects. When central fluid volume is restored acutely by head-out immersion, thirst is attenuated in young subjects only, even though 70% of the plasma volume loss was restored in the older men. This suggests that age differences in thirst arise from changes in the cardiovascular system (i.e., baroreceptor function or responsiveness). In both age groups, fluid intake followed thirst ratings. (Data redrawn from Stachenfeld et al. (33).)]
[ FIGURE 5—A unifying hypothesis proposed by Stachenfeld et al. (33) to explain differences in thirst between older and younger adults. During “normally occurring” dehydration, osmolality increases and blood volume decreases. Young adults are thirstier at a given osmolality because the blood volume deficit is sensed appropriately. Older adults respond to increased osmolality in a similar manner regardless of vascular volume. That is, thirst deficiency in the elderly occurs because of a reduced ability to sense a volume deficit; osmo-regulation is relatively intact. See also Figures 3 and 4.]
... response to repeated dehydrating stimuli also appears to be reduced, which may contribute to a relative inability to expand plasma volume. When age differences are noted in the physiological control systems associated with thirst and satiety, hypovolemia seems to be more closely associated with a decreased thirst sensation. Available evidence suggests that older men and women have a higher osmotic operating point for thirst sensation under normal daily conditions, and a diminished sensitivity to thirst and satiety reflexes arising from unloading (hypovolemia) and loading(hypervolemia) of baroreceptors, respectively.
Children
When exposed to high environmental heat, children are less effective thermoregulators* than adults because of their high surface area/mass ratio, underdeveloped sweating and skin blood flow mechanisms, and other factors (2).
[*Thermoregulation is the ability of an organism to keep its body temperature within certain boundaries, even when the surrounding temperature is very different. ]
Since thermoregulatory capacity in children is closely related to their hydration status, it is particularly important to understand alterations in the thirst mechanism of children that might lead to dehydration. Unfortunately, few studies have been performed that look at this issue from a mechanistic standpoint. Unlike the aging studies noted above, investigators have not examined separate and combined effects of stimulating thirst via hypovolemia and hypertonicity. This is a fruitful area for future research.
Voluntary dehydration in children. As is the case for young adults, children are susceptible to voluntary dehydration. Voluntary dehydration is defined as the lack of complete rehydration after a dehydrating stimulus because of inadequate or lack of prolonged thirst. In a study conducted by Bar-Or et al. (4), boys aged 10–12 yr exercised for 20–25 min, alternating with 20 min of rest, for a total of 3 hours in a hot environment. When allowed free access to 26°C water, the boys progressively dehydrated as the study continued. Mild voluntary dehydration occurs in well-acclimatized children living in tropical climates as well. Nine children (aged 13 ± 2 yr) were tested (28) under four conditions: sun exposure with forced drinking, sun exposure with voluntary drinking, shade with forced drinking, and shade with voluntary drinking. Forced drinking trials were those in which the amount of water (in a bottle at arm’s length at 15–17°C) consumed was the volume estimated to replace body weight losses. The subjects exercised for four 20-min sessions with 25 min of rest in between for a total of 180 min. Cumulative water intake was greater during the forced drinking trials compared with the ad libitum trials and cumulative weight loss was lower. Although thermoregulation was effective, a mild voluntary dehydration was noted. Voluntary water intake for the sun and shade conditions was 53% and 25% of their intake during the “forced”trials, respectively.Influence of drink flavoring on thirst and fluid intake. Palatability or taste of a beverage and drink composition have been shown to play a significant role in promoting fluid intake in adults. This is the case for children as well. Meyer and Bar-Or (16) had children aged 9 to 13 years exercise for 90 min in a hot, dry environment followed by a 30-min recovery, during which time drinks of varying flavors (grape, apple, orange, and water) were given ad *libitum. [*Ad lib: Abbreviation for the Latin "ad libitum" meaning "at pleasure" and "at one's pleasure, as much as one desires, to the full extent of one's wishes." Sometimes seen on a prescription or doctor's order.]
On the basis of visual analog scale ratings, the children’s thirst intensity began to increase after ~100 grams of body weight loss and increased with increasing dehydration. During recovery, however, most of the children voluntarily overhydrated with all the different flavored drinks. Grape and orange intake exceeded that for apple and water. Although grape was the preferred drink throughout the dehydration phase, its desirability did not increase as much as the desirability for orange, apple, and water with increasing dehydration. This indicates that during normally hydrated states, grape is the preferential flavor for children, but in times of dehydration, orange may be more greatly desired. It could be possible, however, that the grape-flavored drink reached a ceiling value for desirability. This study suggests that availability of flavored drinks after exercise-induced dehydration may promote increased fluid intake. However,it should be noted that the magnitude of dehydration in this study (like many pediatric studies) was small, about 290 g or 0.76% of body weight.
Influence of drink composition on thirst and fluid intake. Sweating rate is lower in children than in adults, as is the sodium concentration of the sweat. Therefore, total sodium losses in sweat tend to be lower in children, even when corrected for body mass (16). Inclusion of sodium in replacement drinks promotes drinking and may aid in fluid retention in the vascular space.
To examine the influence of sodium content on thirst and fluid intake in children, Meyer et al. (17,18) studied 9- to 12-yr-old children who were kept euhydrated* [*Normal state of body water content; absence of absolute or relative hydration or dehydration. ... euhydration the normal state of body water content (typically about 40 litres).] while cycling for three intermittent bouts followed by a high-intensity ride to exhaustion in 35°C. During a 30-min recovery period, the subjects were allowed to drink ad libitum one of four as-signed drinks that differed in sodium content. The drinks were sweetened grape-flavored water, grape-flavored 6% CHO with no sodium, grape-flavored 6% CHO with 8.8mEq·L⁻1 sodium, or grape-flavored 6% CHO with 18.5m Eq·L⁻1 sodium. There were no changes in plasma osmolality or sodium regardless of drink composition. Drink composition likewise did not affect drinking behavior during recovery, and volume intake was similar across trials(~200 mL). Perceived thirst and “stomach fullness” were similar across trials. Thus, well-hydrated children (with little thirst drive) show no preference for drinks on the basis of sodium concentration, even after exercise in a warm environment.
However, a follow-up study by the same group (37) again compared drinking responses to unflavored water, grape-flavored water, and grape-flavored water with 6% CHO and18.5 mEq·L⁻1 sodium. Boys aged 9 to 12 yr cycled at 35°C intermittently for a total of 180 min and drinks were available in a chilled bottle for ad libitum consumption without encouragement. Total drink intake by the end of sessions was 44.5% higher with flavored water than with water alone and 91% higher when flavoring, carbohydrate, and sodium were added to the water. In the CHO-Na beverage trials,
fluid intake exceeded fluid loss, whereas in the other two trials dehydration occurred (Fig. 7).
FIGURE 7—Drinking response of boys aged 9 –12 yr during exercise. In children from both temperate and tropical climates, flavoring of water increased consumption over unflavored water. Adding 6% carbohydrate to the flavored water increased intake again compared with plain water. When flavored carbohydrate-electrolyte drinks are available, children rarely experience voluntary dehydration. (Redrawn from data published in Wilk and Bar-Or (37) and Rivera-Brown et al. (27).)
This study shows the importance of both flavor and composition in increasing fluid intake in children. This response is consistent across multiple days of exercise-heat exposure, as this CHO-N a beverage resulted in a positive fluid balance in 67 out of 72 sessions conducted over a 2-weeks period (38).
Finally, in a study conducted by Rivera-Brown et al. (27), twelve 11- to 14-year-old boys indigenous to a tropical climate cycled intermittently outdoors at a wet-bulb globe temperature of 30°C. These tropical natives had higher sweating rates than those measured in children in previous chamber trials. Each boy went through two exercise sessions: one with unflavored water and one with flavored 6% CHO and 18 mmol·L⫺1 Na solution (CHO-Na). They found that the subjects drank 32% more in the CHO-Na session than in the water-only session (Fig. 7). It was also noted that voluntary rehydration during the CHO-Na session resulted in a positive fluid balance, whereas the water resulted in a negative fluid balance (ineffective replacement). A preferred-flavor beverage containing 6% CHO and 18 mmol·L⁻1 Na promotes more drinking than water to help rehydrate children in exercising conditions similar to those of possible outdoor climates. In children, as in adults, it is clear that palatability and drink composition affect the volume of fluids voluntarily consumed during and after dehydrating exercise.
Osmotic thirst in children. Although no mechanistic studies have been performed on thirst stimulation in children, some clues can be gained from comparisons of healthy children with those with cystic fibrosis (CF). CF patients lose large amounts of NaCl in the sweat that would attenuate the increase in plasma osmolality. If plasma hypertonicity were a major drive for thirst, CF children would be expected to report lower thirst sensations and less fluid consumption.This has been demonstrated in a study by Bar-Or et al. (3),despite similar degrees of heat strain in CF patients and normal control children. In a subsequent study (13), addition of 30 mmol·L⫺1 NaCl did not increase voluntary drinking compared with water in such patients. However, when 50 mmol· L⫺1 NaCl was given, voluntary drinking increased and voluntary dehydration was prevented. This lends credence to the importance of osmotic thirst in children.
Conclusion. Children seldom voluntarily dehydrate in activities lasting 45 min or less (Bar-Or, O., personal communication). Flavoring drinks and adding NaCl in the range of ~18 mmol·L⫺1 increases ad libitum fluid intake. Few if any laboratory studies have been performed aimed at elucidating mechanistic differences of thirst in children, that is, examining differences when challenged by hyperosmotic versus hypovolemic stimuli. Data examining oropharyngeal metering in children are also lacking.
PRACTICAL IMPLICATIONS
Clearly, fluid replacement in children and the elderly should not rely on thirst alone. Education about proper hydration is an essential element for these two populations. In older adults, longer time periods should be given for rehydration after dehydration. In children, flavoring and NaCl content of the ingested fluids are important promoters of drinking. However, no specific changes in the composition of currently available carbohydrate-electrolyte drinks are recommended by the sparse data currently available. Neither age group is prone to chronic dehydration as previously suggested in the popular literature.
The authors are indebted to the Gatorade Sports Science Institute for their support of this review and wish to acknowledge the helpful editorial comments and suggestions of Drs. Oded Bar-Or,Gary Mack, Nina Stachenfeld, Bob Murray, and David Lamb.
Studies from the author’s laboratory were supported by National Institutes of Health grants R01-AG07004 and M01-RR10732.
Address for correspondence: W. Larry Kenney, Ph.D., FACSM,Noll Physiological Research Center, 102 Noll Laboratory, Penn State University, University Park, PA 16802; E-mail: w7k@psu.edu.FIGURE 7—Drinking response of boys aged 9–12 years during exercise. In children from both temperate and tropical climates, flavoring of water increased consumption over unflavored water. Adding 6% carbohydrate to the flavored water increased intake again compared with plain water. When flavored carbohydrate-electrolyte drinks are available, children rarely experience voluntary dehydration. (Redrawn from data published in Wilk and Bar-Or (37) and Rivera-Brown et al. (27).)AGE AND THIRST Medicine & Science in Sports & Exercise1531
REFERENCES
1. AGATE,J.The Practice of Geriatrics. London: Heinemann, 1970, p. 41.2.
2. BAR-OR, O. Temperature regulation during exercise in children and adolescents. In: C. G. Gisolfi and D. R. Lamb (Eds.). Perspectives in Exercise Science and Sports Medicine: Youth, Exercise, and Sport,Vol. 2. Carmel, IN: Benchmark Press, 1989, pp. 335–368.3.
3. BAR-OR, O., C. J. BLIMKIE, J.D.HAY, J.D.MACDOUGALL, D. S. WARD, and W. M. WILSON. Voluntary dehydration and heat intolerance in cystic fibrosis. Lancet 339:696–699, 1992.4.
4. BAR-OR, O., O. INBAR, A.ROTHSHTEIN, and H. ZONDER. Voluntary hypohydration in 10- to 12-year-old boys. J. Appl. Physiol. 48:104–108, 1980.5.
5. CROWE, M. J., M. L. FORSLING, B.J.ROLLS, P.A.PHILLIPS, J.G.G.LEDINGHAM, and R. F. SMITH. Altered water excretion in healthy elderly men. Age Ageing 16:285–293, 1987.6.
6. DE CASTRO, J. M. A micro regulatory analysis of spontaneous fluid intake by humans: evidence that the amount of fluid ingestion and its timing is governed by feeding. Physiol. Behav. 43:705–714,1988.7.
7. DE CASTRO, J. M. The relationship of spontaneous macro nutrient and sodium intake with fluid ingestion and thirst in humans. Physiol. Behav. 49:513–519, 1991.8.
8. DE CASTRO, J. M. Age-related changes in natural spontaneous fluid ingestion and thirst in humans. J. Gerontol. 47:P321–P330, 1992.9.
9. FAULL, C. M., C. HOLMES, and P. H. BAYLIS. Water balance in elderly people: is there a deficiency of vasopressin? Age Ageing 22:114–120, 1993.10.
10. FIGARO, M. K., and G. W. MACK. Control of fluid intake in dehydrated humans: role of oropharyngeal stimulation. Am.J. Physiol. 272:R1740–R1746, 1997.11.
11. GISOLFI, C. V., R. W. SUMMERS,H.P.SCHEDL, and T. L. BLEILER. Intestinal water absorption from select carbohydrate solutions in humans. J. Appl. Physiol. 73:2142–2150, 1992.12.
12. KENNEY, W. L., C. G. TANKERSLEY, D.L.NEWSWANGER, D.E.HYDE, and S. M. PUHL. Age and hypohydration independently influence the peripheral vascular response to heat stress. J. Appl.Physiol. 68:1902–1908, 1990.
13. KRIEMER, S., B. WILK,W.SCHURER,W.M.WILSON, and O.BAR-OR. Preventing dehydration in children with cystic fibrosis who exercise in the heat. Med. Sci. Sports Exerc. 31:774–779, 1999.
14.Lo¨WIK,M.R.H.,S.WESTENBRINK,K.F.A.M.HULSHOF,C.KISTE-MAKER, and R. J. J. HERMUS. Nutrition and aging: dietary intake ofapparently healthy elderly. J. Am. Coll. Nutr. 8:347–356, 1989.
15. MACK, G. W., C. A. WESEMAN, G.W.LANGHANS, H.SCHERZER,C. M. GILLEN, and E. R. NADEL. Body fluid balance in dehydrated healthy older men: thirst and renal osmoregulation. J. Appl.Physiol. 76:1615–1623, 1994.
16. MEYER, F., and O. BAR-OR. Fluid and electrolyte loss during exercise: the paediatric angle. Sports Med. 18:4–9, 1994.
17. MEYER, F., O. BAR-OR,D.MACDOUGALL, and G. J. F. HEIGEN-HAUSER. Drink composition and the electrolyte balance of children exercising in the heat. Med. Sci. Sports Exerc. 27:882–887, 1995.
18. MEYER, F., O. BAR-OR,A.SALSBERG, and D. PASSE. Hypohydration during exercise in children: effect on thirst, drink preferences, and rehydration. Int. J. Sports Med. 4:22–35, 1994.
19. MIESCHER, E., and S. M. FORTNEY. Responses to dehydration and rehydration during heat exposure in young and older men. Am.J. Physiol. 257:R1050–R1056, 1989.
20. O’NEILL, P. A., E. B. FARAGHER, I.DAVIES,R.WEARS, K.A.MCLEAN, and D. S. FAIRWEATHER. Reduced survival with increasing plasma osmolality in elderly continuing care patients. Age Ageing 19:68–71, 1990.
21. PHILLIPS, P. A., M. BRETHERTON, C.I.JOHNSTON, and L. GRAY. Reduced osmotic thirst in healthy elderly men. Am. J. Physiol.261:R166–R171, 1991.
22. PHILLIPS, P. A., M. BRETHERTON, J.RISVANIS, D.CASLEY, C.JOHNSTON, and L. GRAY. Effects of drinking on thirst and vasopressin in dehydrated elderly men. Am. J. Physiol. 264:R877–R881, 1993.
23. PHILLIPS, P. A., C. I. JOHNSTON, and L. GRAY. Thirst and fluid intake in the elderly. In: D. J. Ramsay and D. A. Booth (Eds.). Thirst:Physiological and Psychological Aspects. London: Springer-Ver-lag, 1991, pp. 403–411.
24. PHILLIPS, P. A., and B. J. ROLLS. Thirst and dehydration. In: M.Fiatarone-Singh (Ed.). Exercise, Nutrition and the Older Woman:Wellness for Women Over 50. Boca Raton, FL: CRC Press, 2000,pp. 443–452.
25. PHILLIPS, P. A., B. J. ROLLS,J.G.G.LEDINGHAM, and J. J. MORTON.Body fluid changes, thirst and drinking in man during free access to water. Physiol. Behav. 33:357–363, 1984.
26. PHILLIPS, P. A., B. J. ROLLS, M.L.LEDINGHAM, et al. Reduced thirst after water deprivation in healthy elderly men. N. Engl. J. Med.311:753–759, 1984.
27. RIVERA-BROWN, A. M., R. GUTIERREZ, J.C.GUTIERREZ, W.R.FRONTERA, and O. BAR-OR. Drink composition, voluntary drinking,and fluid balance in exercising, trained, heat-acclimatized boys. J. Appl. Physiol. 86:78–84, 1999.
28. RODRIGUEZ-SANTANA, J. R., A. M. RIVERA-BROWN, W.R.FRONTERA, M. A. RIVERA, P.M.MAYOL, and O. BAR-OR. Effect of drink pattern and solar radiation on thermoregulation and fluid balance during exercise in chronically heat acclimatized children. Am.J. Hum. Biol. 7:643–650, 1995.
29. ROLLS, B. J. Homeostatic and non-homeostatic controls of drinking in humans. In: M. J. Arnaud (Ed.). Hydration Throughout Life.
Montrouge, France: John Libbey Eurotext, 1998, pp. 19–28.
30. SCHOORLEMMER, G. H. M., A. K. JOHNSON, and R. L. THUNHORST. Effect of hyperosmotic solutions on salt excretion and thirst in rats. Am. J. Physiol. 278:R917–R923, 2000.
31. SNYDER, M. A., D. W. FEIGAL, and A. L. ARIEFF. Hypernatraemia* in elderly patients: a heterogenous, morbid and iatrogenic^^ entity. Ann. Intern. Med. 107:309–319, 1987.[*Hypernatremia is a common electrolyte problem that is defined as a rise in serum sodium concentration to a value exceeding 145 mmol/L. [1, 2, 3] It is strictly defined as a hyperosmolar condition caused by a decrease in total body water (TBW) relative to electrolyte content. ] [^^iatrogenic,ʌɪˌatrə(ʊ)ˈdʒɛnɪk/adjective/relating to illness caused by medical examination or treatment."drugs may cause side effects which can lead to iatrogenic disease" ]
32. SPANGLER, P. F., T. R. RISLEY, and D. D. BILYEW. The management of dehydration and incontinence in non-ambulatory geriatric patients. J. Appl. Behav. Anal. 17:397–401, 1984.
33. STACHENFELD, N. S., L. DIPIETRO,E.R.NADEL, and G. W. MACK. Mechanism of attenuated thirst in aging: role of central volume* receptors. Am. J. Physiol. 272:R148–R157, 1997.
[*Atrial volume receptors are low pressure baroreceptors that are found in the atria of the heart and carotid arteries.
When these receptors detect a blood volume decrease in the atria, a signal is transmitted from the receptors to the hypothalamus in the brain. The hypothalamus, in turn, increases the production of vasopressin (ADH, AVP, or arginine vasopressin). These receptors also cause a renal vasodilation, resulting in increase of the water amount in the glomerular filtrate which, combined with the increased production of vasopressin by the hypothalamus, will cause water retention in urine. This increases the blood volume, resulting in the increase of blood pressure.]
Am. J. Physiol. 272:R148–R157, 1997.
34. STACHENFELD, N. S., G. W. MACK,A.TAKAMATA,L.DIPIETRO, and E. R. NADEL. Thirst and fluid regulatory responses to hypertonicity in older adults. Am. J. Physiol. 271:R757–R765, 1996.
35. STRICKER, E. M., and J. G. VERBALIS. Hormones and behavior: the biology of thirst and sodium appetite. Am. Sci. 76:261–267, 1988.
36. TAKAMATA, A., T. ITO,Y.KAZUHIRO, et al. Effect of an exercise-heat acclimation program on body fluid regulatory responses to dehydration in older men. Am. J. Physiol. 277:R1041–R1050,1999.
37. WILK, B., and O. BAR-OR. Effect of drink flavor and NaCl on voluntary drinking and hydration in boys exercising in the heat.
J. Appl. Physiol. 80:1112–1117, 1996.
38. WILK, B., S. KRIEMLER,H.KELLER, and O. BAR-OR. Consistency in preventing voluntary dehydration in boys who drink a flavored carbohydrate-NaCl beverage during exercise in the heat.
Int.J. Sports Nutr. 8:1–9, 1998.
39. ZAPPE, D. H., G. W. BELL, H.SWARTZENTRUBER, R.F.WIDEMAN, and W. L. KENNEY. Age and regulation of fluid and electrolyte balance during repeated exercise sessions. Am. J. Physiol. 270:R71–R79, 1996
Influence of Age on Thirst and Fluid Intake (PDF Download Available). Available from: https://www.researchgate.net/publication/11818351_Influence_of_Age_on_Thirst_and_Fluid_Intake [accessed Jun 3, 2017].
turgor; təːɡə, the state of turgidity and resulting rigidity of cells or tissues, typically due to the absorption of fluid. "turgor pressure".
If no dehydration is present, the skin returns quickly to the normal position. With moderate to severe dehydration, decreased skin turgor causes the pinched-up .



No comments:
Post a Comment