About the Author
Dr. Fereydoon Batmanghelidj ( "Batman-ge-lij" ー who did not wish to be licensed for "practice of pharmaceutically oriented and invasive medicine in the U.S.") received formal medical training at St. mary'd Hospital Medical School (London University). He research into the phenomenon of pain and water metabolism of the human body has dictated a paradigm change in the basic understanding of science applied to the practice of medicine. His views are published in scientific journals. The underlying principles of the recommendations in his treatment procedures are the most current knowledge of anatomy and the science of physiology.
Since a highly significant and basic paradigm change is the practice of medicine, in the face of very stiff commercial and professional resistance, will be difficult to institute unless there is a concurrent public educational program to force the change, it has become necessary to begin a highly coordinated public awareness program. The author believes: " To end major diseases in earth within two decades is now a possibility. A paradigm change in the science of medicine will do it, but the public must demand the change. the time to act is now." - 1991, F. Batmanghelidj.
About the Author
Dr. Fereydoon Batmanghelidj ( "Batman-ge-lij" ー who did not wish to be licensed for "practice of pharmaceutically oriented and invasive medicine in the U.S.") received formal medical training at St. mary'd Hospital Medical School (London University). He research into the phenomenon of pain and water metabolism of the human body has dictated a paradigm change in the basic understanding of science applied to the practice of medicine. His views are published in scientific journals. The underlying principles of the recommendations in his treatment procedures are the most current knowledge of anatomy and the science of physiology.
Since a highly significant and basic paradigm change is the practice of medicine, in the face of very stiff commercial and professional resistance, will be difficult to institute unless there is a concurrent public educational program to force the change, it has become necessary to begin a highly coordinated public awareness program. The author believes: " To end major diseases in earth within two decades is now a possibility. A paradigm change in the science of medicine will do it, but the public must demand the change. the time to act is now." - 1991, F. Batmanghelidj.
For production of educational materials for public, under legal advisement, it became necessary to establish Global Health Solutions Inc.*, a legally independent enterprise. This self-treatment manual, How to Deal Simply with Back Pain & Rheumatoid Joint Pain, and the videotape How to Deal with Back Pain are the first of these educational products.
*NOTE: About Us: Global Health Solutions
Global Health Solutions, GHS, a worldwide publishing house, founded and developed by F. Batmagnhelidj, M.D., the world's foremost medical researcher on the medical properties of water, is a center of education for those who prefer to adhere to the logic of the natural and the simple in medicine.
GHS is dedicated to spreading the information of new science in medicine and promoting the public awareness of the hidden wonders of natural, simple, pure water in improving the public health and well-being.
GHS publishes Dr. F. Batmanghelidj¡'s pioneering work on dehydration that identifies different health problems caused by persistent dehydration of the human body - a totally different perspective to the cause and cure of many human diseases until now thought to be incurable.
Dr. B's two decades of research revealed a simple truth that unintentional chronic dehydration can cause diseases; it also demonstrated that many of the chronic degenerative diseases are preventable, and some of them can even be cured by increasing daily water intake. Dr. B's groundbreaking work provides new knowledge and new possibilities for improving and maintaining good health that the public need and deserve to know.
GHS is proud to be the publisher of all of Dr. B's six books in the series of You're Not Sick, You're Thirsty, as well as some of his most informative and inspiring public lectures and seminars in audio-visual formats.
GHS is committed to fulfilling Dr. B's mission - a mission to educate the public about the truth of dehydration so that we will not become unnecessarily over-drugged; to promote the public awareness of the healing powers of water so that we can become healers of our own bodies; to transform the expensive sick-care system so that we can have a more nature-friendly, people-friendly health care system.
LOOK INSIDE THE BOOK, CLICK HERE.
How to Deal with Back Pain and Rheumatoid Joint Pain is a practical manual based on the author's many years of research and numerous clinical observations. The book introduces a new medical technology to treat and prevent back pain and rheumatoid joint pain.
* Learn the vital information on the mechanics behind your spinal column, the role of the disc and its needs for water.
* Learn the simple body movement that will promote fluid circulation in the disc spaces that will result in relief of the back pain and sciatic pain.
* It is simple, safe and inexpensive.
Don't hate yourself for missing out on this information.
The Cell
Let us take a look at the most basic life-generating element in the human body, the cell. The cell is surrounded by a very thin outer "skin" or membrane that protects it from being flooded by unregulated entry of water, salt, sugar, fats and many other elements that constitute the serum solution that is outside the cell wall.
Since the cell is constantly bathed in serum solution, it regulates its intake and output by means of many, many small pumping units. Fluid inside the cells should be neutral, neither too acidic nor too alkaline; it has a pH of 7.4 under normal circumstance. The way this neutral pH maintained is very simple : the cation (cat-i-on) pumps constantly pump out hydrogen ion, which is the acid substance not used by the cell. The entire human body ー nerve tissue, bone, cartilage, ligament, muscle, blood, brain, you name it ー is made up of these tiny cells, each performing this regulation of intake and output of elements to maintain function. Each cell is just like an underwater city, with canal systems and waterways; outside of it, arteries and veins are its highways.
 The skeletal structure displaying various pathologies.
The skeletal structure displaying various pathologies.
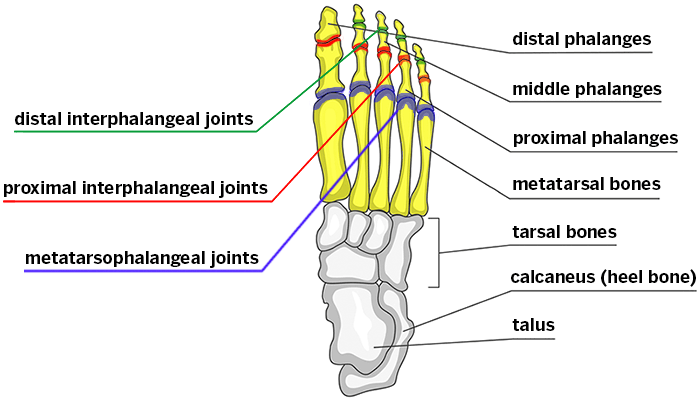
The function of all of the muscles in the lower limb originating below the knee is to move the foot. These muscles insert on any one or several of the 26 bones of the foot.
Bones of the Foot
The 26 bones of the foot, separated into the three main sections of the foot: Forefoot, Midfoot, Hindfoot, is summarized below:
 (From toes to heel) ⇧
Bones of the Right Foot
Distal Phalanges
Middle Phalanges
Proximal Phalanges
(From toes to heel) ⇧
Bones of the Right Foot
Distal Phalanges
Middle Phalanges
Proximal Phalanges
1st Metatarsal
2nd Metatarsal
3rd Metatarsal
4th Metatarsal
5th Metatarsal
Medial Cuneiform
Middle Cuneiform
Lateral Cuneiform
Navicular
Cuboid
CALCANEOCUBOID JOINT
TALONAVICULAR JOINT
Combined articulations make up
the MIDTARSAL JOINT
Talus
Calcaneus


⇧Bones of Right Foot (Lateral View)
Joints of the Foot

The forefoot.
The forefoot consists of five metatarsals starting with the first to the fifth; and five toes, each of which consists of three bones (except for the big toe which consists of two). The bones of
each toe are the proximal phalanx, the middle phalanx, and the distal phalanx (except the big toe which has only proximal and distal). Between each of these bones is a joint which allows for the
movement necessary of each section of the foot.
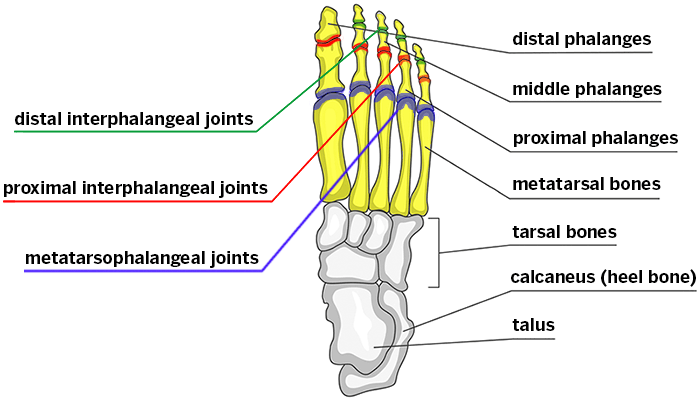
The joints of the forefoot are:
1. MTP joint - metatarsal phalangeal joint - between the metatarsal and the proximal phalanx of the adjacent toe.
2. PIP joint - proximal interphalangeal joint - between the proximal phalanx and the middle phalanx of each toe.
3. DIP joint - distal interphalangeal joint - between the middle phalanx and the distal phalanx of each toe.
4. The big (“great”) toe has only one joint between its two phalanges and therefore this joint is called the great (or “big” ) toe interphalangeal joint.
Metatarsal head is the end of the metatarsals, which articulate with the joints of the adjacent bones (generally used to describe the distal metatarsal head, the portion that articulates with the proximal
phalanx of the adjacent toe.)

The midfoot:
The Midfoot consists of five bones with numerous articular surfaces (surfaces which articulate by
way of joints with other bones).
1. navicular
2. cuboid
3. three cuneiform bones: medial, middle and lateral
Distally, the fourth and fifth metatarsals articulate with the cuboid bone. The first, second and third metatarsals articulate with each of their respective cuneiform bones. Each of these has an
individual joint capsule but all are wrapped in one big capsule as well to form the tarso-metatarsal joint (the “Lis Franc joint”).

 Proximally, the talonavicular and calcaneocuboid joints, together form the combined articulations of the midtarsal joint (of “Chopart”).
Proximally, the talonavicular and calcaneocuboid joints, together form the combined articulations of the midtarsal joint (of “Chopart”).
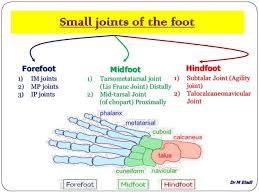
 The Hindfoot
The tibia articulates with the dome of the talus and thereby transmits the forces of the leg to the ankle. This is commonly called the “Tibialtalar joint” or simply the “Ankle joint”. In turn, the
talus articulates with the calcaneus, the main weight-bearing (and the largest) bone of the foot by way of the subtalar joint.
The Hindfoot
The tibia articulates with the dome of the talus and thereby transmits the forces of the leg to the ankle. This is commonly called the “Tibialtalar joint” or simply the “Ankle joint”. In turn, the
talus articulates with the calcaneus, the main weight-bearing (and the largest) bone of the foot by way of the subtalar joint.
 The subtalar joint, known as the “agility joint”, is a key joint in the ankle. It has three surfaces of articulation with three separate facet joints. A great deal of the movement in the ankle happens in this joint - the rest of the movement happens at the tibialtalar joint.
The subtalar joint, known as the “agility joint”, is a key joint in the ankle. It has three surfaces of articulation with three separate facet joints. A great deal of the movement in the ankle happens in this joint - the rest of the movement happens at the tibialtalar joint.
The plantar fascia is an important stabilizer in the foot where a great deal of foot pathology begins. The plantar fascia originates from the plantar surface of the calcaneus and attaches to the plantar
surfaces of the five metatarsal heads and proximal phalanges of the toes. The plantar fascia acts as a major stabilizer of the foot (see diagram). It helps maintain the arch of the foot and is an antipronator. In its function of maintaining the congruity of the relationship between the calcaneus and the metatarsal heads, it resists the torsion movement of the forefoot in relation to the hindfoot during pronation. Most of the eversion of pronation occurs in the mid and forefoot while the calcaneus remains stable in the hindfoot.
http://www.wefixfeet.ca/sites/default/files/anatomyofthefoot.pdf
Human Body Organ Systems
The human body is made up of 11 organ systems that work with one another (interdependantly). These systems include the
1. integumentary system,
2. skeletal system,
3. muscular system,
4. lymphatic system,
5. respiratory system,
6. digestive system,
7. nervous system,
8. endocrine system,
9. cardiovascular system,
10. urinary system, and
11. reproductive systems.
We will briefly discuss the major functions of each organ system below.
1. Integumentary system– (skin, hair, nails) Forms the external body covering and protects deeper tissues from injury. Houses cutaneous receptors, sweat glands, oil glands, and synthesizes vitamin D.
2. Skeletal system– (bones, joints) Supports and protects the body’s organs. Provides a framework muscles use (movement). Bones also store minerals and create blood cells.
3. Muscular system– (skeletal muscles) Maintains posture and produces movement (locomotion). Produces heat.
4. Lymphatic system– (red bone marrow, thymus, lymphatic vessels, thoracic duct, spleen, lymph nodes) Houses white blood cells (lymphocytes) involved in immunity. Returns leaked fluid from blood vessels to the blood and disposes debris within the lymphatic stream.
5. Respiratory system– (nasal cavity, pharynx, larynx, trachea, bronchus, lung) Removes carbon dioxide and continually supplies blood with oxygen. Gaseous exchanges occur in the respiratory system (lungs).
Human Body's 11 organ systems

7. Digestive system– (oral cavity, esophagus, liver, stomach, small intestine, large intestine, rectum, anus) Breaks down food to be absorbed and eliminates indigestible waste.
8. Nervous system– (brain, spinal cord, nerves) Control system of the body, responds to internal and external changes, activates muscles and glands.
9. Endocrine system– (pineal gland, pituitary gland, thyroid gland, thymus, adrenal gland, pancreas, ovary, testis) Glands from the endocrine system secrete hormones that regulate many processes like growth, metabolism, and reproduction.
10. Cardiovascular system– (heart, blood vessels) The heart pumps blood and blood vessels transport it. Blood carries oxygen, carbon dioxide, nutrients, waste and more throughout the body.
Urinary system– (kidney, ureter, urinary bladder, urethra) Eliminates nitrogenous wastes from the body. Regulates acid-base, electrolyte and WATER balance of blood.
11. Reproductive systems
MALE (prostate gland, penis, testis, scrotum, ductus deferens)
FEMALE (Mammary glands, ovary, uterus, vagina, uterine tube)
The main function of the reproductive system is to produce offspring. Sex hormone and sperm are produced by the male testes. Male ducts and glands help deliver the sperm. Ovaries produce female sex hormones and eggs. Other female reproductive structures serve as sites of fertilization and development. For instance, the mammary glands produce milk for the newborn.

 This educational and preventive treatment manual gives you easy-to-use techniques for relieving chronic back pain and rheumatoid joint pain. This new approach to prevention and treatment of back pain is simpler, inexpensive, less dangerous and more effective.
-- Learn the vital information on the mechanics behind your spinal column, the role of the disc and its needs for water
-- Learn the simple body movement that will promote fluid circulation in the disc spaces the twill result in relief of back and sciatic pain.
This educational and preventive treatment manual gives you easy-to-use techniques for relieving chronic back pain and rheumatoid joint pain. This new approach to prevention and treatment of back pain is simpler, inexpensive, less dangerous and more effective.
-- Learn the vital information on the mechanics behind your spinal column, the role of the disc and its needs for water
-- Learn the simple body movement that will promote fluid circulation in the disc spaces the twill result in relief of back and sciatic pain.
Dr. F. Batmanghelidj ( "Batman-ge-lij"- who did not wish to be licensed for "practice of pharmaceutic-ally oriented and invasive medicine in the U.S.") received formal medical training at St. Mary's Hospital Medical School (London University) . His research into the phenomenon of pain and water metabolism of the body has dictated a paradigm change in the basic understanding of science applied to the practice of medicine. His views are published in scientific journals. The underlying principles of the recommendations in his treatment procedures are the most current knowledge of anatomy and the science of physiology.
How to Deal with Back Pain and Rheumatoid Joint Pain is a practical manual based on the author’s many years of research and numerous clinical observations. The book introduces a new medical technology to treat and prevent back pain and rheumatoid joint pain. * Learn the vital information on the mechanics behind your spinal column, the role of the disc and its needs for water. * Learn the simple body movement that will promote fluid circulation in the disc spaces that will result in relief of the back pain and sciatic pain. * It is simple, safe and inexpensive. Don’t hate yourself for missing out on this information. Dr. Batmanghelidj received his formal medical education at St. Mary’s Hospital Medical School of London University. He provides for the layman a clear and comprehensive book on the origins of chronic pain. His clinical and scientific research exposes, for the first time, that recurring “chronic pains” are a signal system of the body indicating severe general or local dehydration. Most of these pains can be relieved simply by drinking enough water. Instead, however, the patient often receives costly pharmaceutical medications which treat rather than cure. In this book, back pain and rheumatoid joint pain as indicators of local chronic dehydration are explained. The mechanisms involving the important role of water in holding the spinal column together are discussed. Based on years of detailed study of the human anatomy and the science of physiology, Dr. Batmanghelidj has devised a new exercise approach for the successful hydration of the disc core, the retraction of the displaced discs, and immediate relief of pain, even sciatica. These exercises are clearly explained and demonstrated, and may be the only way to save yourself from the surgeon’s knife. This book is unlike any other “how-to” book on the market. It is an instructive presentation about the very simple way of finding comfort and relief from two of the most commonly occurring pains of the body low back pain and rheumatoid joint pain.
The Foundation For The Simple In Medicine
In 1983, the Foundation for the Simple in Medicine, a charitable medical research (think tank) foundation, was founded to establish grounds for a change in the present fundamental understanding of the basis on which all human applied research has been done. The present basic assumption in practice of medicine (paradigm) is that it is the physico-chemical properties of ions ( "i-ons" are the purest form of the basic elements, such as sodium, potassium, calcium, magnesium, etc.) that regulate the water intake of the human body, and that the substance we call "water," the solvent of the body, performs a passive role to these basic elements and everything else that is dissolved in the same solvent.
Why? Because early in research , it was recognized that solutes (substances that are dissolved in the body fluids) are highly reactive substances. Clinical experience has shown that this assumption cannot be complete , because the human body can become dehydrated as we progress in age. The Foundation for the Simple in Medicine holds the opinion that since the sensor regulators to ion exchanges that regulate the water movement in the human body are proteins, and proteins by nature are obedient in the presence of water, the more free water there is around them, the more efficiently these proteins function. It therefore follows that it must be water that ultimately regulates its own intake.
Clinically , this view can be validated by the fact that people who do not acknowledge thirst even though dehydrated, after a few days of regulating their water intake on a "forced voluntary" basis, will rediscover their thirst sensation -- their body's craving for water. The Foundation for the Simple in Medicine is making another statement which follows the logic of the previous view: Since all functions of the human body are water-dependent, let us revise our approach to medical treatment procedures; let us recognize a primary water regulatory role for the neurotransmitter systems that has been recognized to be involved in the water intake mechanisms of the body. In the medical condition where these systems are being chemically manipulated to make the patient "better," let us try to satisfy the natural urge of these systems for water before there is any chemical interference with their systems' other natural emergency regulatory functions. The systems recognized for water regulation for the body are : serotonergic (which regulates the calcium movement of the cell, and pain registration among many other functions, histaminergic (which regulates cat-i-ons --cations are the basic elements that carry a positive electric charge-- exchange in the cell, also recognized in many other functions, induction of pain and allergy) and renin-angiotensin (which is stimulated into activity by the two previous systems independently and possibly simultaneously, manipulated in hypertension.)
To introduce its ideas into the practice of medicine all over the world, The Foundation for the Simple in Medicine has begun the publication of its scientific views in its own Science in Medicine Simplified (Sci. Med.Simplified), which is periodically printed and distributed to research centers and medical libraries in different parts of the world.
Our Invitation to Worldwide Readers
" Let us lobby together and ask the scientists in medicine to begin the evaluation of the statements dictated by the new paradigm that recognizes the regulatory and reactive hydrolytic functions of water in the human body. Under the new paradigm , you can rest assured , the practice of medicine will become a much gentle preventive, as well as curative , physiological approach to early disease emergence , before the damage is done.
We are most interested in hearing your reactions to this book and invitation, and about results success or relief you may achieve by following the suggestions and exercises presented herein.
If you follow the program and recommendations and do not experience relief, we would like to hear about that as well. the comments of physicians and other health-care professionals will be particularly appreciated.
Please sent comments, reactions, and suggestions to:
Back Pain
P.O.Box 3189
Falls Church, Virginia 22043, USA.
All responses will be held in strictest confidence.
Back Pain, Disc Displacement,
Rheumatoid Joint Pain : Water and Exercise
This educational preventive-treatment manual will deal with chronic back pain and rheumatoid joint pain in language as simple as possible , although the impact of what is being said will eventually fill volumes of written material. The reader is advised not to judge the value of this book by its simplicity of presentation, but should try to evaluate the essence of what is being said. Justification of confused views will always produce voluminous verbiage, particularly when held views have to have an application appeal for the people who are at the receiving end, and if it eventually will mean expensive surgical interferences.
If we are to prevent decompensation and/or achieve relief from pain of disc displacement , we have to make sure that our human body is optimally hydrated so that water can leave the main blood circulatory systems and hydrate the disc core; also, from the front angle of the intervertebral spaces is kept widely open, until corrective restitution to the physical properties and position of the disc have taken place: How do we do this?

 You are encouraged to read this book in its entirety; however, a preliminary reading of the first part of the manual will clearly illuminate how it is possible to alleviate the pain and anxiety of back discomfort , mild or excruciating. The more detailed part of the manual should then be read to revise and learn more about the physiology of pain, the cell, the nerves sensitive to pain ; referred pain and/or muscle weakness caused by a prolapsed intervertebral disc; weight and motion and their effect; the foot and its arches; special points about pelvic anatomy and distribution of forces; the relationship of the disc to the vertebra; the disc and its functions; and the cartilage and the joints.
Simple exercises and hydrolic treatment (regulated water intake) are carefully explained.
Here, then, is a guide to the care and preventive treatment of back pain and disc displacement , as well as rheumatoid joint pain.
Chronic Pain : What Does It Signify?
This book started as a simple address of back pain, which, as everyone knows, is a devastating chronic pain of the human body. as my research at the Foundation (The Foundation for the Simple in Medicine) into the phenomenon of pain has steadily progressed, I realized that this book would be incomplete if some explanation on the "other" chronic joint pain of the body -- rheumatoid arthritis -- was not included. After all , most back pain originates at the vertebral joints, and if book was to be a grass-roots approach to pain, rheumatoid joint pain is an equally devastating condition that also deserved discussion. The fundamental explanations about the origin of rheumatoid joint pain are equally simple, and, at the onset, it is even more simply treatable than back pain.
A news item in the 31st July,1990 Health Section of The Washington Post gave me sufficient emotional shock to re-structure this book, which was at that time already in the printer's hands.
A 47-year-old child psychiatrist had been suffering from severe rheumatoid arthritis for some time. She had been given the customary medications until she had developed addiction, apparently, and the combination of addiction and pain had totally incapacitated her. She had a daughter of 17, who was brain-damaged and asthmatic, and a son who was bright. The stress in the family setting had become so great that even the housekeeper suffered a heart attack. The psychiatrist's husband, himself a doctor and a prominent cancer researcher, eventually found the situation unbearable enough that he took the lives of his wife and two children and then committed suicide.
To my mind, this tragedy --- along with similar , daily-occurring tragedies, --- stemmed from a most absurd ignorance and the "ostrich" policy of those involved in the politics of medicine. The scientific knowledge that can offer simple solutions to major health problems --- most particularly , at a preventable stage that would not cause severe genetic damage -- does exist.
For the innocent and trusting sick to benefit from the solutions offered within the science of physiology, medicine will need a change of stand by some key policy-makers and the government administrators of health who support the present commercial attitude of the health-care industry; medical professionals will need to give support to alternative ideas and the more plausible science-based solutions to the health problems of the sick. This change of attitude might not serve the profit motivations of the industrial and commercial arms of the health-care institutions, but it should be remembered that simple, nature-serving solutions to major public health problems are less costly to the society they are obligated to serve.
You are encouraged to read this book in its entirety; however, a preliminary reading of the first part of the manual will clearly illuminate how it is possible to alleviate the pain and anxiety of back discomfort , mild or excruciating. The more detailed part of the manual should then be read to revise and learn more about the physiology of pain, the cell, the nerves sensitive to pain ; referred pain and/or muscle weakness caused by a prolapsed intervertebral disc; weight and motion and their effect; the foot and its arches; special points about pelvic anatomy and distribution of forces; the relationship of the disc to the vertebra; the disc and its functions; and the cartilage and the joints.
Simple exercises and hydrolic treatment (regulated water intake) are carefully explained.
Here, then, is a guide to the care and preventive treatment of back pain and disc displacement , as well as rheumatoid joint pain.
Chronic Pain : What Does It Signify?
This book started as a simple address of back pain, which, as everyone knows, is a devastating chronic pain of the human body. as my research at the Foundation (The Foundation for the Simple in Medicine) into the phenomenon of pain has steadily progressed, I realized that this book would be incomplete if some explanation on the "other" chronic joint pain of the body -- rheumatoid arthritis -- was not included. After all , most back pain originates at the vertebral joints, and if book was to be a grass-roots approach to pain, rheumatoid joint pain is an equally devastating condition that also deserved discussion. The fundamental explanations about the origin of rheumatoid joint pain are equally simple, and, at the onset, it is even more simply treatable than back pain.
A news item in the 31st July,1990 Health Section of The Washington Post gave me sufficient emotional shock to re-structure this book, which was at that time already in the printer's hands.
A 47-year-old child psychiatrist had been suffering from severe rheumatoid arthritis for some time. She had been given the customary medications until she had developed addiction, apparently, and the combination of addiction and pain had totally incapacitated her. She had a daughter of 17, who was brain-damaged and asthmatic, and a son who was bright. The stress in the family setting had become so great that even the housekeeper suffered a heart attack. The psychiatrist's husband, himself a doctor and a prominent cancer researcher, eventually found the situation unbearable enough that he took the lives of his wife and two children and then committed suicide.
To my mind, this tragedy --- along with similar , daily-occurring tragedies, --- stemmed from a most absurd ignorance and the "ostrich" policy of those involved in the politics of medicine. The scientific knowledge that can offer simple solutions to major health problems --- most particularly , at a preventable stage that would not cause severe genetic damage -- does exist.
For the innocent and trusting sick to benefit from the solutions offered within the science of physiology, medicine will need a change of stand by some key policy-makers and the government administrators of health who support the present commercial attitude of the health-care industry; medical professionals will need to give support to alternative ideas and the more plausible science-based solutions to the health problems of the sick. This change of attitude might not serve the profit motivations of the industrial and commercial arms of the health-care institutions, but it should be remembered that simple, nature-serving solutions to major public health problems are less costly to the society they are obligated to serve.
 The human gastrointestinal tract refers to the stomach and intestine, and sometimes to all the structures from the mouth to the anus.
The major organs of the human gastrointestinal system.
The human gastrointestinal tract refers to the stomach and intestine, and sometimes to all the structures from the mouth to the anus.
The major organs of the human gastrointestinal system.
The major organs of the human gastrointestinal system are identified in this drawing. The upper gastrointestinal tract consists of the esophagus, stomach, and duodenum. The lower gastrointestinal tract includes most of the small intestine and all of the large intestine. According to some sources, it also includes the anus.
Upper Gastrointestinal Tract
The upper gastrointestinal tract consists of the esophagus, stomach, and duodenum. The exact demarcation between upper and lower can vary. Upon gross dissection, the duodenum may appear to be a unified organ, but it is often divided into two parts based upon function, arterial supply, or embryology.
The upper gastrointestinal tract includes the:
Esophagus, the fibromuscular tube that food passes through—aided by peristaltic contractions—the pharynx to the stomach.
Stomach, which secretes protein-digesting enzymes called proteases and strong acids to aid in food digestion, before sending the partially digested food to the small intestines.
Duodenum, the first section of the small intestine that may be the principal site for iron absorption.
Lower Gastrointestinal Tract
The lower gastrointestinal tract includes most of the small intestine and all of the large intestine. According to some sources, it also includes the anus.
 The small intestine has three parts:
The small intestine has three parts:
Duodenum: Here the digestive juices from the pancreas (digestive enzymes) and the gallbladder (bile) mix together. The digestive enzymes break down proteins and bile and emulsify fats into micelles. The duodenum contains Brunner's glands that produce bicarbonate, and pancreatic juice that contains bicarbonate to neutralize hydrochloric acid in the stomach.
Jejunum: This is the midsection of the intestine, connecting the duodenum to the ileum. It contains the plicae circulares and villi to increase the surface area of that part of the GI tract.
Ileum: This has villi, where all soluble molecules are absorbed into the blood ( through the capillaries and lacteals).
The large intestine has four parts:
1.Cecum, the vermiform appendix that is attached to the cecum.
2.Colon, which includes the ascending colon, transverse colon, descending colon, and sigmoid flexure. The main function of the colon is to absorb water, but it also contains bacteria that produce beneficial vitamins like vitamin K.
3.Rectum.
4.Anus.
The ligament of Treitz is sometimes used to divide the upper and lower GI tracts.
 Processes and Functions of the Digestive System
Processes and Functions of the Digestive System
Digestion is necessary for absorbing nutrients from food and occurs through two processes: mechanical and chemical digestion.
The Digestive System
The proper functioning of the gastrointestinal (GI) tract is imperative for our well being and life-long health. A non-functioning or poorly-functioning GI tract can be the source of many chronic health problems that can interfere with your quality of life.
Here is a look at the importance of two main functions of the digestive system: digestion and absorption.
Digestion
The gastrointestinal tract is responsible for the breakdown and absorption of the various foods and liquids needed to sustain life. Many different organs have essential roles in the digestion of food, from the mechanical breakdown of food by the teeth to the creation of bile (an emulsifier) by the liver.
Bile production plays a important role in digestion: it is stored and concentrated in the gallbladder during fasting stages, and discharged to the small intestine. Pancreatic juices are excreted into the digestive system to break down complex molecules such as proteins and fats.
Absorption
Absorption occurs in the small intestines, where nutrients directly enter the bloodstream.
Each component of the digestive system plays a special role in these complimentary processes. The structure of each component highlights the function of that particular organ, providing a seamless anatomy to keep our body fueled and healthy.
Components of the Digestive System
The digestive system is comprised of the alimentary canal, or the digestive tract, and other accessory organs that play a part in digestion—such as the liver, the gallbladder, and the pancreas. The alimentary canal and the GI tract are terms that are sometimes used interchangeably.
The alimentary canal is the long tube that runs from the mouth (where the food enters) to the anus (where indigestible waste leaves). The organs in the alimentary canal include the mouth (the site of mastication), the esophagus, the stomach, the small and large intestines, the rectum, and the anus. From mouth to anus, the average adult digestive tract is about thirty feet (30') long.
Processes of Digestion
Food is the body's source of fuel. The nutrients in food give the body's cells the energy they need to operate. Before food can be used it has to be mechanically broken down into tiny pieces, then chemically broken down so nutrients can be absorbed.
In humans, proteins need to be broken down into amino acids, starches into sugars, and fats into fatty acids and glycerol. This mechanical and chemical breakdown encompasses the process of digestion.
To recap these twin processes:
Mechanical digestion: Larger pieces of food get broken down into smaller pieces while being prepared for chemical digestion; this process starts in the mouth and continues into the stomach.
Chemical digestion: Several different enzymes break down macromolecules into smaller molecules that can be absorbed. The process starts in the mouth and continues into the intestines.
Moistening and Breakdown of Food
Digestion begins in the mouth. A brain reflex triggers the flow of saliva when we see or even think about food. Enzymes in saliva then begin the chemical breakdown of food; teeth aid in the mechanical breakdown of larger food particles.
Saliva moistens the food, while the teeth masticate the food and make it easier to swallow. To accomplish this moistening goal, the salivary glands produce an estimated three liters of saliva per day.
Amylase, the digestive enzyme found in saliva, starts to break down starch into simple sugars before the food even leaves the mouth. The nervous pathway involved in salivary excretion requires stimulation of receptors in the mouth, sensory impulses to the brain stem, and parasympathetic impulses to salivary glands. Once food is moistened and rolled and ready to swallow, it is known as a bolus.
Swallowing and the Movement of Food
For swallowing to happen correctly a combination of 25 muscles must all work together at the same time. Swallowing occurs when the muscles in your tongue and mouth move the bolus into your pharynx. Bolus (from Latin bolus, ball)is a small rounded mass of a substance, especially of chewed food at the moment of swallowing.
"mucin holds the particles of food together in a ball or bolus" Mucin is a glycoprotein constituent of mucus.
"mucin is secreted by the salivary glands"
The pharynx, which is the passageway for food and air, is about five inches (5") long—a remarkably small space. A small flap of skin called the epiglottis closes over the pharynx to prevent food from entering the trachea, which would cause choking. Instead, food is pushed into the muscular tube called the esophagus. Waves of muscle movement, called peristalsis, move the bolus down to the stomach.
While in the digestive tract, the food is really passing through the body rather than being in the body. The smooth muscles of the tubular digestive organs move the food efficiently along as it is broken down into easily absorbed ions and molecules.
Large-scale Breakdown in the Stomach
Once the bolus reaches the stomach, gastric juices mix with the partially digested food and continue the breakdown process. The bolus is converted into a slimy material called chyme.

Major digestive hormones
There are at least five major digestive hormones in the gut of mammals that help process food through chemical digestion in the gall bladder, duodenum, stomach, and pancrease. These hormones are cholecystokinin, gastric inhibitory polypeptide, motilin, secretin, and gastrin.
This (see above) is a drawing of the digestive system. This shows the five major digestive hormones in the gut of mammals that help process food through chemical digestion in the gall bladder, duodenum, stomach, and pancrease. These hormones are cholecystokinin, gastric inhibitory polypeptide, motilin, secretin, and gastrin.
The stomach is a muscular bag that maneuvers food particles, mixing highly acidic gastric juice and powerful digestive enzymes with the chyme to prepare for nutrient absorption in the small intestine. Stimulatory hormones such as gastrin and motilin help the stomach pump gastric juice and move chyme. The complex network of hormones eventually prepares chyme for entry into the duodenum, the first segment of the small intestine.
Absorption in the Small Intestine
During absorption, the nutrients that come from food (such as proteins, fats, carbohydrates, vitamins, and minerals) pass through the wall of the small intestine and into the bloodstream. In this way nutrients can be distributed throughout the rest of the body. The small intestine increases surface area for absorption through tiny interior projections, like small fingers, called villi.
Waste Compaction in the Large Intestine
In the large intestine there is resorption of water and absorption of certain minerals as feces are formed. Feces are the waste parts of the food that the body passes out through the anus.
Organs of the Digestive System
The organs of the digestive system can be divided into upper and lower digestive tracts. The upper digestive tract consists of the esophagus, stomach, and the small intestine; the lower tract includes all of the large intestine, the rectum, and anus.
The human body uses a variety of mental and physiological cues to initiate the process of digestion. Throughout our gastrointestinal (GI) tract, each organ serves a specific purpose to bring our food from the plate to a digestible substance from which nutrients can be extracted.
The Digestive Tube
Our digestive system is like a long tube, with different segments doing different jobs. The major organs within our digestive system can be split into two major segments of this tube: the upper gastrointestinal tract, and the lower gastrointestinal tract.
The Upper Gastrointestinal Tract
The upper gastrointestinal, or GI, tract is made up of three main parts:
The esophagus.
The stomach.
The small intestine.
 The Lower Gastrointestinal Tract
The Lower Gastrointestinal Tract
The lower GI tract contains the remainder of the system:
The large intestine.
The rectum.
The anus.
The exact dividing line between upper and lower tracts can vary, depending on which medical specialist is examining the GI tract.
Food Breakdown and Absorption: The Upper GI Tract
When we take a bite of food, the food material gets chewed up and processed in the mouth, where saliva begins the process of chemical and mechanical breakdown. The chewing process is also known as mastication.
When we mix up food with saliva, the resulting mushy wad is called a bolus. The bolus gets swallowed, and begins its journey through the upper gastrointestinal tract.
The Esophagus
The upper GI tract begins with the esophagus, the long muscular tube that carries food to the stomach. The throat cavity in which our esophagus originates is known as the pharynx. As we swallow, the bolus moves down our esophagus, from the pharynx to the stomach, through waves of muscle movement known as peristalsis. Next the bolus reaches the stomach itself.
The Stomach
The stomach is a muscular, hollow bag that is an important part of the upper GI tract. Many organisms have a variety of stomach types, with many segments or even multiple stomachs. As humans, we have only one stomach.
Here our bolus gets mixed with digestive acids, furthering breakdown of the bolus, and turning the bolus material into a slimy mess called chyme. The chyme moves on into the small intestine, where nutrients are absorbed.
The Small Intestine
The small intestine is an impressive digestive tube, spanning an average of 20 feet in length. The twists and turns of the small intestine, along with tiny interior projections known as villi, help to increase the surface area for nutrient absorption.
This snaking tube is made up of three parts, in order from the stomach:
The duodenum.
The jejunum.
The ileum.
As the chyme makes its way through each segment of the small intestine, pancreatic juices from the pancreas start to break down proteins. Soapy bile from the liver, stored in the gallbladder, gets squirted into the small intestine to help emulsify—or break apart—fats.
Now thoroughly digested, with its nutrients absorbed along the path of the small intestine, what remains of our food gets passed into the lower GI tract.
Waste Compaction and Removal: The Lower Gastrointestinal Tract
The Large Intestine (Colon)
Following nutrient absorption, the food waste reaches the large intestine, or colon. The large intestine is responsible for compacting waste material, removing water, and producing feces—our solid-waste product.
Accessory organs like the cecum and appendix, which are remnants of our evolutionary past, serve as special pockets at the beginning of the large intestine. The compacted and dried-out waste passes to the rectum, and out of the body through the anus. Healthy gut bacteria in the large intestine also help to metabolize our waste as it finishes its journey.
Enteric Nervous System
The enteric nervous system (ENS) is a subdivision of the autonomic nervous system (ANS) that directly controls the gastrointestinal system.
The gastrointestinal (GI) system has its own nervous system, the enteric nervous system (ENS). Neurogastroenterology is the study of the enteric nervous system, a subdivision of the autonomic nervous system (ANS) that directly controls the gastrointestinal system. The ENS is capable of autonomous functions such as the coordination of reflexes.
Although it receives considerable innervation from the autonomic nervous system, it can and does operate independently of the brain and the spinal cord. The ENS consists of some 100 million neurons, one-thousandth of the number of neurons in the brain, and about one-tenth the number of neurons in the spinal cord. The enteric nervous system is embedded in the lining of the gastrointestinal system.
Ganglia of the ENS
The neurons of the ENS are collected into two types of ganglia:
1.The myenteric (Auerbach's) plexus, located between the inner and outer layers of the muscularis externa.
2.The submucosal (Meissner's) plexus, located in the submucosa.
The Myenteric Plexus
The myenteric plexus is mainly organized as a longitudinal chains of neurons. When stimulated, this plexus increases the tone of the gut as well as the velocity and intensity of its contractions. This plexus is concerned with motility throughout the whole gut. Inhibition of the myenteric system helps to relax the sphincters—the muscular rings that control the flow of digested food or food waste.
The Submucosal Plexus
The submucosal plexus is more involved with local conditions and controls local secretion and absorption, as well as local muscle movements. The mucosa and epithelial tissue associated with the submucosal plexus have sensory nerve endings that feed signals to both layers of the enteric plexus. These tissues also send information back to the sympathetic pre-vertebral ganglia, the spinal cord, and the brain stem.
 Neural control of the gut.
An illustration of neural control of the gut wall by the autonomic nervous system and the enteric nervous system.
Neural control of the gut.
An illustration of neural control of the gut wall by the autonomic nervous system and the enteric nervous system.
Function and Structure of the ENS
The enteric nervous system has been described as a second brain. There are several reasons for this. For instance, the enteric nervous system can operate autonomously. It normally communicates with the central nervous system (CNS) through the parasympathetic (e.g., via the vagus nerve) and sympathetic (e.g., via the prevertebral ganglia) nervous systems. However, vertebrate studies show that when the vagus nerve is severed, the enteric nervous system continues to function.
In vertebrates, the enteric nervous system includes efferent neurons, afferent neurons, and interneurons, all of which make the enteric nervous system capable of carrying reflexes and acting as an integrating center in the absence of CNS input. For instance, the sensory neurons report mechanical and chemical conditions, while the motor neurons control peristalsis and the churning of intestinal contents through the intestinal muscles. Other neurons control the secretion of enzymes.
The enteric nervous system also makes use of more than 30 neurotransmitters, most of which are identical to the ones found in the CNS, such as acetylcholine, dopamine, and serotonin. More than 90% of the body's serotonin is in the gut, as well as about 50% of the body's dopamine, which is currently being studied to further our understanding of its utility in the brain.
The enteric nervous system has the capacity to alter its response depending on factors such as bulk and nutrient composition. In addition, the ENS contains support cells that are similar to the astroglia of the brain, as well as a diffusion barrier around the capillaries that surround the ganglia, which is similar to the blood–brain barrier of the cerebral blood vessels.
Regulation of ENS Function
The parasympathetic nervous system is able to stimulate the enteric nerves in order to increase enteric function. The parasympathetic enteric neurons function in defecation and provide a rich nerve supply to the sigmoid colon, the rectum, and the anus.
Conversely, stimulation of the enteric nerves by the sympathetic nervous system will inhibit enteric function and capabilities. Neurotransmitter secretion and direct inhibition of the enteric plexuses cause this stall in function. If the gut tract is irritated or distended, afferent nerves will send signals to the medulla of the brain for further processing.
Gastrointestinal Reflex Pathways
The digestive system functions via a system of long reflexes, short reflexes, and extrinsic reflexes from gastrointestinal (GI) peptides that work together.
Food in the Digestive System
The digestive system has a complex system of food movement and secretion regulation, which are vital for its proper function. Movement and secretion are regulated by long reflexes from the central nervous system (CNS), short reflexes from the enteric nervous system (ENS), and reflexes from the gastrointestinal system (GI) peptides that work in harmony with each other.
In addition, there are three overarching reflexes that control the movement, digestion, and defecation of food and food waste:
1.The enterogastric reflex.
2.The gastrocolic reflex.
3.The gastroileal reflex.
Long and Short Reflexes
Long reflexes to the digestive system involve a sensory neuron that sends information to the brain. This sensory information can come from within the digestive system, or from outside the body in the form of emotional response, danger, or a reaction to food.
These alternative sensory responses from outside the digestive system are also known as feedforward reflexes. Emotional responses can also trigger GI responses, such as the butterflies in the stomach feeling when nervous.
Control of the digestive system is also maintained by enteric nervous system (ENS), which can be thought of as a digestive brain that helps to regulate motility, secretion, and growth. The enteric nervous system can act as a fast, internal response to digestive stimuli. When this occurs, it is called a short reflex.
Three Main Types of Gastrointestinal Reflex
1.The enterogastric reflex is stimulated by the presence of acid levels in the duodenum at a pH of 3–4 or in the stomach at a pH of 1.5. When this reflex is stimulated, the release of gastrin from G-cells in the antrum of the stomach is shut off. In turn, this inhibits gastric motility and the secretion of gastric acid (HCl). Enterogastric reflex activation causes decreased motility.
2.The gastrocolic reflex is the physiological reflex that controls the motility, or peristalsis, of the gastrointestinal tract. It involves an increase in motility of the colon in response to stretch in the stomach and the byproducts of digestion in the small intestine. Thus, this reflex is responsible for the urge to defecate following a meal. The small intestine also shows a similar motility response. The gastrocolic reflex also helps make room for food in the stomach.
3.The gastroileal reflex is a third type of gastrointestinal reflex. It works with the gastrocolic reflex to stimulate the urge to defecate. This urge is stimulated by the opening of the ileocecal valve and the movement of the digested contents from the ileum of the small intestine into the colon for compaction.
 Peristalis
The gastrocolic reflex is one of a number of physiological reflexes that control the motility, or peristalsis, of the gastrointestinal tract.
GI Peptides that Contribute to Gastrointestinal Signals
GI peptides are signal molecules that are released into the blood by the GI cells themselves. They act on a variety of tissues that include the brain, the digestive accessory organs, and the GI tract.
Peristalis
The gastrocolic reflex is one of a number of physiological reflexes that control the motility, or peristalsis, of the gastrointestinal tract.
GI Peptides that Contribute to Gastrointestinal Signals
GI peptides are signal molecules that are released into the blood by the GI cells themselves. They act on a variety of tissues that include the brain, the digestive accessory organs, and the GI tract.
The effects range from excitatory or inhibitory effects on motility and secretion, to feelings of satiety or hunger when acting on the brain. These hormones fall into three major categories:
1.The gastrin family.
2.The secretin family.
3.A third family that is composed of the hormones that do not fit into either of these two families.