HIRA (Hazard Identification and Risk Assessment) :
The purpose of this guideline is to provide a systematic and objective approach to assessing
hazards and their associated risks that will provide an objective measure of an identified hazard as well as provide a method to control the risk. It is one of the general duties as prescribed under the Occupational Safety and Health Act 1994 (Act 514) for the employer to provide a safe workplaces to their employees and other related person.
Term And Definitions:
Hazard means a source or a situation with a potential for harm in terms of human injury or ill health, damage to property, damage to the environment or a combination of these.
Hazard control means the process of implementing measures to reduce the risk associate with a hazard.
Hierarchy of control means the established priority order for the types of measures to be used to control risks.
Hazard identification means the identification of undesired events that lead to the materialization of the hazard and the mechanism by which those undesired events could occur.
Risk means a combination of the likelihood of an occurrence of a hazardous event with specified period or in specified circumstances and the severity of injury or damage to the health of people, property, environment or any combination of these caused by the event.
Risk assessment means the process of evaluating the risks to safety and health arising from hazards at work.
Risk management means the total procedure associated with identifying a hazard, assessing the risk, putting in place control measures, and reviewing the outcomes.
Basic Concepts:
What is risk?
Risk is something that we as individuals live with on a day-to-day basis. People are constantly making decisions based on risk. Simple decision in daily life such as driving, crossing the road and money investment all imply an acceptance risk. Risk is the combination of the likelihood and severity of a specified hazardous event occurring.
In mathematical term, risk can be calculated by the equation - Risk = Likelihood x Severity
Where,
Likelihood is an event likely to occur within the specific period or in specified circumstances
and,
Severity is outcome from an event such as severity of injury or health of people, or damage to property, or insult to environment, or any combination of those caused by the event.
Planning And Conducting Of Hira :
The purpose of HIRA are as follows:-
a. to identify all the factors that may cause harm to employees and others (the hazards);
b. to consider what the chances are of that harm actually be falling anyone in the circumstances of a particular case and the possible severity that could come from it (the risks); and
c. to enable employers to plan, introduce and monitor preventive measures to ensure
that the risks are adequately controlled at all times.
HIRA activities shall be plan and conducted :
a) for situation :
i. where hazard appear to pose significant threat;
ii. uncertain whether existing controls are adequate; or/and
iii. before implementing corrective or preventive measures.
b) by organization intending to continuously improve OSH Management System. It should be the duty of the employer to assign a trained personnel to lead a team of employees associated with one particular process or activity to conduct HIRA.
Process of HIRA
Process of HIRA requires 4 simple steps :
(a) classify work activities;
(b) identify hazard;
(c) conduct risk assessment (analyze and estimate risk from each hazard), by calculating or estimating -
i. likelihood of occurrence, and
ii. severity of hazard;
(d) decide if risk is tolerable and apply control measures (if necessary).
Flow chart for HIRA process
Classify work activities →Consultation ( between Employer and Employees)→Identify Hazards → Risk Assessment → Prepare Risk Control Action Plan ( if necessary) → Implement →(review /loop back to Identify Hazards).
Classify work activities:
Classify work activities in accordance with their similarity, such as :
1. geographical or physical areas within/outside premises;
2. stages in production/service process;
3. not too big e.g. building a car;
4. not too small e.g. fixing a nut; or
5. defined task e.g. loading, packing, mixing, fixing the door.
Hazard identification:
The purpose of hazard identification is to highlight the critical operations of tasks, that is, those tasks posing significant risks to the health and safety of employees as well as highlighting those hazards pertaining to certain equipment due to energy sources, working conditions or activities performed. Hazards can be divided into three main groups, health hazards, safety hazards, and environmental hazards.
Health hazards:
An occupational health hazard is any agent that can cause illness to an individual. A health hazard may produce serious and immediate (acute) affects, or may cause long-term(chronic) problems. All or part of the body may be affected. Someone with an occupational illness may not recognize the symptoms immediately. For example, noise-induced hearing loss is often difficult for the affected individual to detect until it is well advanced. Health hazards include chemicals (such as battery acid and solvents), biological hazards (such as bacteria, viruses, dusts and molds), physical agents (energy sources strong enough to harmthe body, such as electric currents, heat, light, vibration, noise and radiation) and work design (ergonomic) hazards.
Safety hazards:
A safety hazard is any force strong enough to cause injury, or damage to property. An injury caused by a safety hazard is usually obvious. For example, a worker may be badly cut. Safety hazards cause harm when workplace controls are not adequate.
Some examples of safety hazards include, but are not limited to:
• slipping/tripping hazards (such as wires run across floors);
• fire hazards (from flammable materials);
• moving parts of machinery, tools and equipment (such as pinch and nip points);
• work at height (such as work done on scaffolds);
• ejection of material (such as from molding);
• pressure systems (such as steam boilers and pipes);
• vehicles (such as forklifts and trucks);
• lifting and other manual handling operations; and
• working alone.
Environmental hazards:
An environmental hazard is a release to the environment that may cause harm or deleterious effects. An environmental release may not be obvious. For example, a worker who drains a glycol system and releases the liquid to a storm sewer may not be aware, of the effect on the environment. Environmental hazards cause harm when controls and work procedures are not followed.
Hazard identification technique:
The employer shall develop a hazard identification and assessment methodology taking into account the following documents and information :
• any hazardous occurrence investigation reports;
• first aid records and minor injury records;
• work place health protection programs;
• any results of work place inspections;
• any employee complaints and comments;
• any government or employer reports, studies and tests concerning the health and safety of employees;
• any reports made under the regulation of Occupational Safety and Health Act, 1994
the record of hazardous substances; and
• any other relevant information.
The hazard identification and assessment methodology:
The hazard identification and assessment methodology shall include:
a. Steps and time frame for identifying and assessing the hazards. One must define the steps for the identification of hazards and a time frame for this identification. The following information should be included :
i) who will be responsible for the identification: for example, it may be the work place health and safety committee, or an individual or individuals appointed.by the committee;
ii) the way in which the identification reports are processed: for example, they may be compiled and processed by the committee, or by individuals appointed by the committee:
iii) the identification time frame: for example, the identification of hazards for
workshop A must be completed in December, for workshop B in April and for workshop C in November.
b. The keeping of a record of the hazards.
After having identified the hazards, one must establish and maintain an identification record, either in print or electronic format.
c. A time frame for reviewing and, if necessary, revising the methodology.
The date for the review of the identification: for example, the review of the identification method will be carried out every three years.
To complete hazard identification, one can use techniques to identify hazards. Some examples of techniques include, but are not limited to:
i. work place inspections;
ii. task safety analysis or job hazard analysis;
iii. preliminary investigations;
iv. potential accident factors;
v. failure analysis;
vi. accident and incident investigations.
It is in your interest to adopt your own process and your own identification techniques so that they match one management procedures and the size of business. In fact, the identification method may vary depending on the size of the work place.
Analyze and estimate risk:
Risk is the determination of likelihood and severity of the credible accident/event sequences in order to determine magnitude and to priorities identified hazards. It can be done by qualitative, quantitative or semi quantitative method.
A qualitative analysis uses words to describe the magnitude of potential severity and the likelihood that those severity will occur. These scales can be adapted or adjusted to suit the circumstances and different descriptions may be used for different risks. This method uses expert knowledge and experience to determine likelihood and severity category.
In semi-quantitative analysis, qualitative scales such as those described above are given values. The objective is to produce a more expanded ranking scale than is usually achieve in qualitative analysis, not to suggest realistic values for risk such as is attempted in quantitative analysis.
Quantitative analysis uses numerical values (rather than the descriptive scales used in qualitative and semi-quantitative analysis) for both severity and likelihood using data from a variety of sources such as past accident experience and from scientific research. Severity may be determined by modeling the outcomes of an event or set of events, or by extrapolation from experimental studies or past data. Severity may be expressed in terms of monetary, technical or human impact criteria, or any of the other criteria. The way in which severity and likelihood are expressed and the ways in which they are combined to provide a level of risk will vary according to the type of risk and the purpose for which the risk assessment output is to be used.
In this guidelines qualitative and semi quantitative method uses as an example.
Likelihood of an occurrence:
This value is based on the likelihood of an event occurring. You may ask the question “How many times has this event happened in the past?” Assessing likelihood is based worker experience, analysis or measurement. Likelihood levels range from “most likely” to “inconceivable.” For example, a small spill of bleach from a container when filling a spray bottle is most likely to occur during every shift. Alternatively, a leak of diesel fuel from a secure holding tank may be less probable.
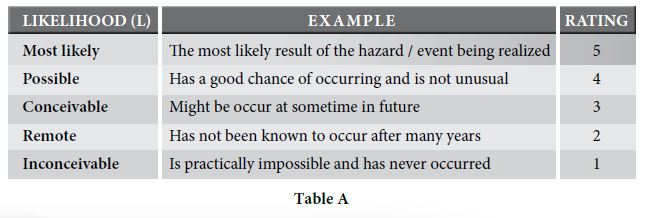
Table A indicates likelihood using the following values:
Table A indicates likelihood using the following values:
Severity of hazard:
Severity can be divided into five categories.
Severity are based upon an increasing level of severity to an individual’s health, the environment, or to property. Table B indicates severity by using the following table :
( Table B )
SEVERITY (S): Catastrophic,
EXAMPLE (E): Numerous fatalies, irrecoverable property damage and productivity,
RATING (R): 5.
SEVERITY (S): Fatal
EXAMPLE (E): Approximately one single fatality, major property damage if hazard is realized
RATING (R): 4
SEVERITY (S): Serious
EXAMPLE (E): Non-fatal injury, permanent disability
RATING (R): 3
SEVERITY (S): Minor
EXAMPLE (E): Disabling but not permanent injury
RATING (R): 2
SEVERITY (S): Negligible
EXAMPLE (E): Minor abrasions, bruises, cuts, first aid type injury
RATING (R): 1
Risk assessment :
Risk can be presented in variety of ways to communicate the results of analysis to make decision on risk control. For risk analysis that uses likelihood and severity in qualitative method, presenting result in a risk matrix is a very effective way of communicating the distribution of the risk throughout a plant and area in a workplace.
Risk can be calculated using the following formula:
L x S = Relative Risk
L = Likelihood
S = Severity
An example of risk matrix (Table C) is shown below:
To use this matrix, first find the severity column that best describes the outcome of risk.Then follow the likelihood row to find the description that best suits the likelihood that the severity will occur. The risk level is given in the box where the row and column meet.
The relative risk value can be used to prioritize necessary actions to effectively manage work place hazards. Table D determines priority based on the following ranges:
Hazards assessed, as “High Risk” must have immediate actions, to resolve risk to life safety and or the environment. Individuals responsible for required action, including follow up must be clearly identified. A further detail risk assessment method may require such as quantitative risk assessment as means of determine suitable controls measures.
Control:
Definition: Control is the elimination or inactivation of a hazard in a manner such that the hazard does not pose a risk to workers who have to enter into an area or work on equipment in the course of scheduled work.
Hazards should be controlled at their source (where the problem is created). The closer a control to the source of the hazard is the better. This method is often referred to as applying engineering controls. If this does not work, hazards can often be controlled along the path to the worker, between the source and the worker. This method can be referred to as applying administrative controls. If this is not possible, hazards must be controlled at the level of the worker through the use of personal protective equipment (PPE), although this is the least desirable control.
Selecting a suitable control:
Selecting a control often involves:
a. evaluating and selecting short and long term controls;
b. implementing short-term measures to protect workers until permanent controls can be put in place; and
c. implementing long term controls when reasonably practicable.
For example, suppose a noise hazard is identified. Short-term controls might require workers to use hearing protection. Long term, permanent controls might remove or isolate the noise source.
Types of Control:
At the source of the hazard
a. Elimination - Getting rid of a hazardous job, tool, process, machine or substance is perhaps the best way of protecting workers. For example, a salvage firm might decide to stop buying and cutting up scrapped bulk fuel tanks due to explosion hazards.
b.Substitution - Sometimes doing the same work in a less hazardous way is possible.For example, a hazardous chemical can be replaced with a less hazardous one.Controls must protect workers from any new hazards that are created.
Engineering control:
a. Redesign - Jobs and processes can be reworked to make them safer. For example,containers can be made easier to hold and lift.
b. Isolation - If a hazard cannot be eliminated or replaced, it can some times be isolated, contained or otherwise kept away from workers. For example, an insulated and air-conditioned control room can protect operators from a toxic chemical.
c. Automation - Dangerous processes can be automated or mechanized. For example, computer- controlled robots can handle spot welding operations in car plants. Care must be taken to protect workers from robotic hazards.
d. Barriers - A hazard can be blocked before it reaches workers. For example, special curtains can prevent eye injuries from welding arc radiation. Proper equipment guarding will protect workers from con tacting moving parts.
e. Absorption - Baffles can block or absorb noise. Lockout systems can isolate energy sources during repair and maintenance. Usually, the further a control keeps a hazard away from workers, the more effective it is.
f. Dilution - Some hazards can be diluted or dissipated. For example,ventilation systems can dilute toxic gasses before they reach operators.
Administrative controls:
a. Safe work procedures - Workers can be required to use standardized safety practices. The employer is expected to ensure that workers follow these practices. Work procedures must be periodically reviewed with workers and updated.
b. Supervision and training – Initial training on safe work procedures and refresher training should be offered. Appropriate supervision to assist workers in identifying possible hazards and evaluating work procedures.
c. Job rotations and other procedures can reduce the time that workers are exposed to a hazard. For example, workers can be rotated through jobs requiring repetitive tendon and muscle movements to prevent cumulative trauma injuries. Noisy processes can be scheduled when no one is in the workplace.
d. Housekeeping, repair and maintenance programs - Housekeeping includes cleaning, waste disposal and spill cleanup. Tools, equipment and machinery are less likely to cause injury if they are kept clean and well maintained.
e. Hygiene - Hygiene practices can reduce the risk of toxic materials being absorbed by workers or carried home to their families. Street clothing should be kept in separate lockers to avoid being contaminated by work clothing. Eating areas must be segregated from toxic hazards. Eating should be forbidden in toxic work areas. Where applicable, workers should be required to shower and change clothes at the end of the shift.
Personal protective equipment:
Personal protective equipment (PPE) and clothing is used when other controls measures are not feasible and where additional protection is needed. Workers must be trained to use and maintain equipment properly. The employer and workers must understand the limitations of the personal protective equipment. The employer is expected to require workers to use their equipment whenever it is needed. Care must be taken to ensure that equipment is working properly. Otherwise, PPE may endanger a workers health by providing an illusion of protection.
Monitoring controls:
The effectiveness of controls must be checked regularly. Evaluate and monitor hazard controls during inspections, routine maintenance, and other activities.
Ask the following questions –
a. have the controls solved the problem?
b. is any risk to workers posed by the controls contained?
c. are all new hazards being identified?
d. are significant, new hazards appropriately controlled?
e. are accident reports being analyzed?
f. are any other measures required?
Document control activities to track their effectiveness, if necessary re-evaluate hazards and implement new control measures.
Safe work procedures:
Through the completion of a Job Hazard Analysis, sometimes hazards are identified and cannot be eliminated or engineered out of a particular task. Safe Work Procedures are step by step instructions that allow workers to conduct their work safety when hazards are present. A Safe Work Procedure identifies the materials and equipment needed, and how and when to use them safety.
Safe Work Procedures are generally prepared for -
a. critical high risk jobs where accidents have or could result in severe injuries;
b. hazardous work where accidents occur frequently;
c. new or altered tasks have been introduced;
d. new equipment has been added to a process;
e. a job that requires many detailed tasks;f. where two or more workers required for a job, and each must perform specific
tasks simultaneously; and
g. specific tasks are done infrequently.
Safe Work Procedures must include:
a. regulatory requirements;
b. necessary personal protective equipment;
c. required training;
d. worker responsibilities;
e. specific sequence of steps to follow to complete the work safely;
f. required permits; and
g. emergency procedures.
An example of a task that requires the development of a safe work procedure is confined space entry. Individuals who must work within confined spaces must ensure that safe work procedures are developed and followed to maximize life safety.
Personal protective equipment (PPE):
Personal protective equipment means any equipment which is intended to be worn or held by a person at work and which protects him against one or more risks to his health or safety and any additional accessory designed to meet that objective;
PPE is usually chosen to provide protection appropriate to each of type of hazard present. There are specifications for the types of PPE used for protecting an individual’s head, eyes, footwear, limb and body, fire retardant clothing, respiratory, hearing, and personal flotation devices.
It may also include required apparel for example when traffic hazards are present high
visible and distinguishable “vests must be worn”
Documenting HIRA:
Responsibility and accountability
Proper management of hazards sporadically identified in the workplace can be done through effective process. Ultimately, the individual or team who identified the hazard must ensure proper communication of the hazard to the appropriate workplace authority (manager, department head, or designated person). Each HIRA must be fully documented. The HIRA form must be completed by the HIRA team and signed by the in charge personnel of the area. Departments responsible for the hazards and their control are required to maintain all records of assessments for at least 3 years. (In some cases, legislative requirements will determine the minimum time to retain records).
The appropriate authority is responsible for ensuring that effective and timely controls are applied to the hazard and communicating the results back to the originator. Management or employer must endorse and approve the HIRA results. Employer must communicate all HIRA to employees, monitor the follow up action and keep the records. The HIRA Form (Link below the page, click here) is an example to document the HIRA process.
Documenting process:
Instructions to team leader and persons conducting HIRA :
1. complete HIRARC Form. It is recommended to use a single form for each work process;
2. record the names and designation of HIRAC team members;
3. outline the process workflow and indicate in the form under ‘process/ location column;
4. list all activities ( routine and non-routine) for each work process under the “Work Activity” column;
5. identify the hazards associated with each activity and record in “Hazard” column;
6. determine the effect of each hazard identified and record in “Effect” column;
7. record any existing hazard control measures;
8. determine likelihood (L) from Table A and severity (S) from Table B for eachhazard. Assign P and C rating in respectively column. The existing control measures should be take into consideration while determine (L) and (S);
9. by using Risk Matrix ( Table C and D ) assign one risk and record in “Risk” column;
10. based on the risk assigned, recommend appropriate risk control measures ( see Table D);
11. assign a suitable person to implement the recommended risk control and indicate the follow up action date and status;
12. repeat the HIRA for other activities and process;
13. conduct another round of HIRA after control measures have been implemented;
and
14. review HIRA for every three years or whenever there are changes in process or
APPENDIX A
Examples of Workplace Hazards:
The Hazard Identification listed is to assist in the identification of hazards in the work place. This table provides some additional explanation of the meaning of the hazard classifications.
WORK ENVIRONMENT
Adequate Access : Refers to adequate access to, from and within the workplace.
Air Conditioning: Refers to the uncontaminated air in the work space.
Confined Space: Means enclosed work spaces where people normally do not work (defined in standards)
Temperature Extremes: a) Heat, This includes contact with hot objects, hyperthermia, fire (Non explosions)
b) Cold, This includes contact with cold objects and hypothermia
Lighting: Refers to adequate illumination for the particular work being done
Mental Stress: Includes bullying, workplace violence, shift work, excessive work loads
Dehydration: Adequate water supply for the individuals while working
ENERGY

