Mark Donegan, of Redwood Valley, California,
says, "I'm fidgety because of pain; my body's
telling me to move, so I do it everywhere on the
bus, sitting around with friends,wherever I am."
Donegan, 36, is recovering from a very painful
back problem that nearly crippled him, a
herniated inter-vertebral disk in the lumbar
spine. He weaned himself off heavy medications
offered by physicians and chose instead to heal
himself through natural movement, the key
element in self-healing.
Moving in a natural way frees you. It is well-
known in movement science that the skilled
performer has more degrees of freedom
(movement choices) than the novice. When you
look at a film of Fred Astaire and Ginger
Rogers dancing, you feel their looseness, ease
and pleasure in movement. It says a lot about
our culture that they had to work hard to make
it second nature to move easily. As they dance,
you see that their muscles work only as hard as
appropriate and don't substitute for the work of
other muscles (the principle of isolation).
Without tensing up the abdominals, they move
loosely from their center (the navel area). It's
much less effortful, energy-costly and wearing
than the "normal" movement patterns most of us
exhibit, which eventually create chronic health
problems.
Athletes and dancers don't necessarily move
naturally; when they use the body as a tool, they
block out a sense of its problems and needs.
Natural movement comes out of kinesthetic
awareness, a deep, subtle sense of movement-of
breath, energy, blood and other fluids throughout
the body, of joints finding their full range in all
planes, of muscles becoming supple, strong and
balanced. You become aware of the body's
specific need for movement at any given time.
Natural movement healsㅡit increases circulation,
reduces inflammation, creates strength,
endurance and a sense of well-being, and
nurtures every part of the body, including the
joints. Helping the client restore natural
movement is essential in working with joint and
spine problems.
Unfortunately, most people move in an
unbalanced, constricted way. This kind of
movementㅡpatterns of overuse, under-use and
misuseㅡis damaging to the joints, including
those of the spine. Doing more of it in the name
of "exercise" will only make you worse.
We suggest reviewing the article, "Movement is
Life," (Issue #60, March/April 1996); those
exercises and principles are helpful for people
with back problems.
A back problem years in the making
When Donegan was 29, his job required him to
climb up and jump down to fetch items from
grocery stockrooms many times a day. "We were
expected to move fast," he said. He woke up one
morning feeling that his left leg didn't want to
move. A chiropractor diagnosed herniated disk
(also known as disk prolapse or slipped disk), a
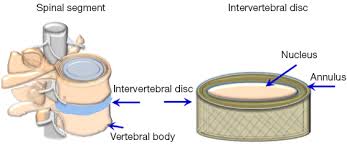
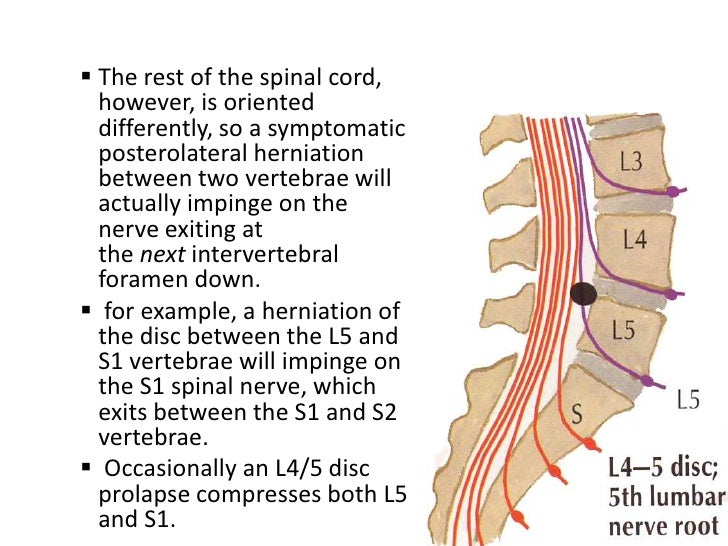
complication of degenerative disk disease. Like
cartilage, intervertebral disks in the spinal
column are believed by physicians to degenerate
inevitably, beginning at early adulthood. As a
complication, the disk may herniate or rupture. A
strong ligament keeps it from bulging directly
backward, so it moves posterolaterally, where it
may compress or stretch a spinal nerve root.

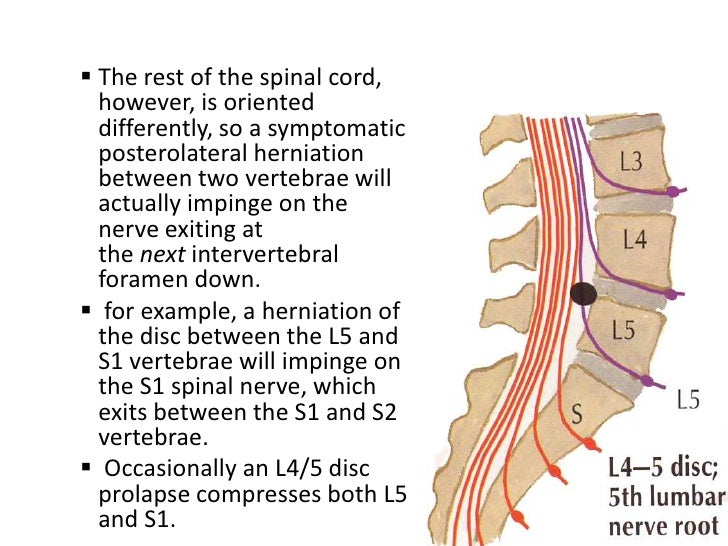
Posterolateral: situated on the side and towards
the back of the body. The result is radiating pain,
muscle weakness and sensory losses, always
along the distribution of the spinal nerve. This is
actually one form of sciatica, which can also
begin with compression further down the nerve.
Most prevalent in young men, herniated disk is
rare after middle age, because the disk has lost a
lot of its mass.
Four months of chiropractic treatment only
aggravated the problem. Donegan tried physical
therapy, and it worsened again, until muscle
spasm and pain prevented movement in the leg
altogether.
Two surgeries brought only temporary respite.
In the first operation, part of the disk and of the
bony arch around the spinal cord were trimmed
away; in the second, more of the disk was
removed and two vertebrae were fused together.
After the second surgery, new symptoms came
onㅡnumbness in the left leg, high blood pressure
, irregular heart rate, bowel and bladder
problems. The right leg had been the anchor for
crutch walking; now he lost sensation and
movement in it, too.
"I was looking at a wheelchair next," Donegan
said. "I was depressedㅡmy whole world was
falling apart. The pain gave me nausea and
vomiting. Let me tell you about extreme pain.
You can take it for a day and it's okay. Two days,
and you start getting tired of it, but on the third
day, you don't have anything left. You're not you
anymore."
Another surgeon told Donegan he could remove
the rest of the damaged disk and stabilize the
region with bone transplants and internal braces
and screws. There would be a new source of pain,
however, from the braces. The surgery restored
his ability to walk but left his back swollen and
painful, and "I had nothing left, no will,"Donegan
said. At a pain clinic in Mendocino, California,
Donegan began working with massage therapist
Audrey Ferrell, who practices neuromuscular
therapy. Ferrell gave him massage and movement
exercises. Gradually his pain abated enough that
he could resume his favorite activity, bicycling.
''I gave the doctor back all of his prescription
pain medications; the only thing I kept was over-
the-counter ibuprofen." A year later, Ferrell
brought him to Meir Schneider. " Meir glanced at
me and told me where my pain was," Donegan
recalls.
While Schneider's evaluation seemed fast and
effortless to Donegan, he used, as always, the
method he teaches students: start with
observations of the client walking both forward
and backward, sitting, climbing stairs and doing
other functional tasks. Overall, Schneider says he
assesses stiffness vs. fluidity in the movement of
each body segment; these are issues with many
health problems. The key is isolation, or
independent movement of each body segment.
"In the extreme case," he says, "paralyzed people
have a concept of 'legs' that needs to be
differentiated; they've forgotten that their legs
can move separately from each other. Without
isolation, you have stiffness.
"Often, with back problems like Mark's,"
Schneider says, "the way one has used the legs
throughout life creates lower back damage.
Mark's knees never fully extend as he walks. He
pushes himself from the upper backㅡ there is
too much forward lean. At the time, he held his
head forward and his shoulders forward and up;
this has improved. Bicycling fit right into this
dynamic posture and aggravated it. Mark's back
is poorly organized, with extreme stiffness in the
thoracic paraspinals and weakness,
comparatively, above and below.

⇧Thoracic Paraspinal Muscle Location and Trigger Points
The Thoracic Paraspinal muscles run lengthwise, parallel to the spine. There are actually two layers of muscle that lie one on top of the other. Because these muscles attach to the vertebrae, or bones of the spine, they can cause problems with spinal misalignment and damage to the intervertebral discs.
The pain of Trigger Points in the Thoracic Paraspinal muscles often feels like it originates in the spine itself. The muscles feel hard and rigid, causing stiffness and decreased movement. It often feels as though the entire back is in spasm, which should respond to treatment with heat and superficial massage. When these treatments do not decrease the pain and spasm, Trigger Points are more likely the cause. Extreme tension in these muscles can lead to scoliosis, or a curvature of the spine.
Due to the close proximity of these muscles with the spine and nerves, Trigger Points in these muscles can also refer pain that mimics problems with organs of the chest and abdomen, such as appendicitis, kidney stones, angina, and lung problems.

Thoracic Paraspinal Stretch ⇧
1. Sit in a chair to stabilize hips.
2. Cross arms at mid forearm, and slowly roll forward, until a stretch is felt
3. Hold for 10-15 seconds.
4. Repeat three times, at least three times daily.
"His face and neck hold a lot of unresolved
emotionㅡjaw locked, sternodeidmastoids and
anterior neck generally very tight. His
abdominals are also extremely stiff. His stiff
areas-anterior neck, anterior and posterior chest,
and abdominal dominate his every movement.
"Mark is strong, fast and capableㅡhe's spent
years weightlifting and wrestling. Unfortunately,
being beefed up makes it harder to clear up
movement imbalances; you've invested that
much more in bad movement patterns.
''With movement imbalances, muscles ate
working in packs-big, insensate blocks, where a
group of proximal muscles tense up to 'help'
inappropriately with the work of a distal muscle.
You may see a psoas / pectorals /
stemocleidomastoid/scalene block like Mark's.
Or your client may have a gluteal/hamstring/
paraspinal/shoulder block, coupled with weak
neck and face, a pattern often seen in near-
sightedness. Or you may see an arched lower
back, protruding chest, with overworked upper
trapezius, lower pectorals, rhomboids and
paraspinals; this pattern goes with farsightedness.
Massage therapists need to carefully identify the
client's whole block."
Shortly after the dynamic posture evaluation,
Schneider's massage begins; it is a major
evaluative tool. "I observe the client's breathing
habits, generally and specifically.
People breathe into an area that is being
massaged; areas where this is delayed are
problematic. Mark's breathing was very
shallow, in the chest mostly, with effortful
exhalations. He didn't breathe at all into the
back. And there were, as I expected, arthritic
and fused joints in the lumbar area.
"I saw that Mark's problems started a long time
before he ever had symptoms. Too many people
look at the end resultㅡthe herniated disk in
Mark's case-of a lifelong movement problem as
if this symptom were the real problem you have
to solve, but it's not. Mark learned early on that
he has to fight for survival; it's in every move he
makes (Mark is a survivor of childhood physical
abuse). The problem may have started with
psychological armoring. It wasn't the job-related
jumping that hurt his back: it was the stiffness in
his jumping. As his pain developed, Mark may
have physiologically splinted against it
(tightened up muscles to shore up an area the
body perceives as weak or threatened),
intensifying his muscle spasms or adding more.
To heal himself, Mark was going to have to
change his movement patterns, and this was
going to create changes at every level of his being."
Physical therapy sees essentially two kinds of
muscle imbalances involved in lower back pain
ㅡtoo much lumbar curve (hyperlordotic) or too
little (flat lower back). They may apply the
classic testㅡhave the patient stand against a
wall and see how many hands' widths he or she
can fit into the lumbar curve-one is normal,
zero or two are problematic. The patient is
then asked to do a standing forward bend and
backbend and describe how each changes the
pain. If it lessens or radiates less, this is the
therapeutic direction for movementㅡpain in the
flat lower back is relieved by backbending; in the
hyperiordotic lower back, by forward bending.
Two leaders in the rehabilitation of backs have
lent their names to these diagnoses/regimen the
Williams protocol is predominantly a spinal
flexion program for hyperlordotic backs; the
MacKenzie, spinal extension for flat low backs.
Schneider says this is useful, as fir as it goes.
Carol Gallup thinks the Williams MacKenzie
distinction is often under-emphasized in the
holistic health community. "A few years ago,
during physical therapy school, I worked briefly
with a young woman with serious lower back
pain, radiating down the legs, with movement
and sensory losses in the legs. Kendra's back
pain began after she allowed a friend who
happened to be a holistic health practitioner to
work with her for a few months to 'correct' her
posture; before that she had had no problem.
This practitioner believed, on the basis of his
training, that the normal lumbar curve was
unhealthy, and that every lower back should be
flat. He did indeed flatten out her lumbar curve
ㅡand created a serious back problem for his
client.
"I see two morals in this story-first, the old
saying, 'if it ain't broke, don't fix it.' Second,
listen to the bioengineers and biomechanics.
They're telling us that the incredible ability of
the back to withstand the stresses we subject it
to every day is caused in part by its shape-
essentially, it's a spring, with the resiliency of a
spring, and it needs the normal amount of
kyphosis* in the upper back and the normal
amount of lordosis in the lower back.
[*Kyphosis (from Greek κυφός kyphos, a hump) is an abnormally excessive convex kyphotic curvature of the spine as it occurs in the cervical, thoracic and sacral regions. (Abnormal inward concave lordotic curving of the cervical and lumbar regions of the spine is called lordosis.)

Hunchback / Kyphosis⇧]
*
⇧ *Lordosis is defined as an excessive inward curve of the spine. It differs from the spine's normal curves at the cervical, thoracic, and lumbar regions, which are, to a degree, either kyphotic (near the neck) or lordotic (closer to the low back).]

So when I met Kendra she had a 'MacKenzie'
back. I gave Kendra some standing and other
[types of] backbends, and her pain immediately
started to lessen and centralize (radiate less), a
sure sign that backbending was an important
direction to take with her therapy.
"I myself happen to tend in the opposite
direction, hyperlordoticㅡa 'Williams' back. I've
found that I do best if, for every six or eight
spinal flexion exercises, I do two or three spinal
extensions. Bear in mind also that serious lower
back pain can occur gram for clients with spine,
joint and when the lower back curve is normal
ㅡthe client may still have muscle tightness,
muscle spasm, very limited mobility."
With the Williams protocol, physical therapists tend to automatically add exercises to strengthen
the abdominals. We know someone who had such severe back pain
that he was admitted to the hospital; a physical therapist looked at his chart and said, "You'll have to strengthen those abdominals; you've got a muscle imbalance causing all that pain." To prove her point, she casually poked at his abdomenㅡand then looked shocked. The patient was a rugby player with magnificent abdominals. He was indeed hyperlordotic, but those strong abdominals weren't correcting it.
Why not? Schneider feels that the problem in
unbalanced movement patterns lies with the
nervous system predominantly and the muscles
only secondarily. Thus, strengthening the
underused muscles alone or in conjunction with
spinal flexion or extension exercises will not
correct the problem. "The brain ignores muscles
in areas it regards as unsupported," he explains.
"'Support' is good mobility in the muscles, not
brute strength; Mark, for example, is very strong
but stiff in the thoracic back, and his brain registers
this as nonsupport and tends to ignore muscles
above it." Schneider's view is at odds with that of
chiropractors and physical therapists, who routinely
make use of lumbar belts, believing they support
the lower back by immobilizing it.
"Hyperflexibility is also seen by the brain as nonsupport-if your client is pathologically loose-jointed, congenitally or from bad stretching programs, there's compensatory muscle tightness."
We need to interfere with the neural habit of
overusing some muscle groups, as if they are the
only muscles it is natural to work, and ignoring
others. A good program for clients with spine,
joint and many other problems involves serious reprogramming. Most of us have immobile toes, for example, from walking in shoes on cement sidewalks, so that our toes and feet didn't develop a pattern of pleasurable sensorimotor interaction with the ground; we can create such a pattern by walking and running on a beach or grassy surface. This is importantㅡstiff feet and calves contribute stiffness to every other joint in the body. And we can interfere with other rigidities in our walk by walking and running backwards. Coordination exercises are very helpful. We can explore the full range of motion of our joints, with movements that take us through many planes (we tend to live in the sagittal, or forward/backward, plane). Massage is essential, since it breaks adhesions and creates new sensory input to the brain, sending it the message that muscles can be soft and mobile. And it is essential for clearing up muscle spasms. Rolling on the floor or the ground is especially helpful, recruiting side muscles that are usually ignored.
We've used the general terms "stiffness", "fluidity,"
and "immobility" purposely when talking about
evaluating movement; these are fairly easy
distinctions to make, visually and through touch.
Later, the evaluator can note muscle spasms or
limited range of motion at the joint. Schneider
found limited joint mobility in Donegan's lumbar
spine and habitual muscle spasm in his psoas,
pectorals, serratus anterior, intercostals, scalenes
and sternocleidomastoid.
"More natural ways of moving-muscles doing only their own work, not adding unnecessary effort, what we call isolationㅡcan't fully take hold until habitual muscle spasm is gone. And it goes away slowly, very slowly, over time. You can clear it up in the sessionㅡwith Self-Healing Neurological Massage (a light-pressure, very vigorous vibrating touch that is a cross between brisk shaking of the muscle and tapotement), tapotement, deep tissue massage, breathing exercisesㅡand the client
walks out much looser, feeling great, thinking
you're wonderful. But the dynamic posture and
the lack of awareness that put it there didn't go away. The client will go home and torque or overload or suddenly strain the back, and the pain may return in full force, and unless you've educated them about the process, they may think the session was a failure. You need to loosen them up and get them doing the movement exercises that teach the brain how to isolate, how to move naturally. There's a long transition period with ups and downs as the new adaptations start, and then eventually they're complete and the spasm is gone."
Donegan was already on a one-hour daily exercise regimen of exercycle workouts, standing lateral and forward bends, knee bends, and stretches for the groin, hamstrings, and calvesㅡ"the standard ones for back pain, on printed sheets that you get from the physical therapist and the chiropractor," Donegan recalls. "They were teaching me movements, trying to figure out bow to get my legs going again, and it wasn't helping. Meir taught me how to move. He pointed out places I was
holding myself; I had an immediate knowledge
that the movements he gave me would release
that area and that release there was the key.
Every exercise improved a symptom."
The regimen that Schneider gave Donegan is described below because it is helpful with his pattern of stiffness and muscle tension, and above all, because it is helping him develop kinesthetic awareness so that he can sense for himself the movements that his body needs. No one program is universally helpful; this one should be looked at in the light of the principles we have discussed.
Exercises to reprogram for soft, fluid movement
The exercises need to be repeated many times; the
effect on the nervous system is slow and
cumulative. All rotations should be done in both
directions.
Seated: First, rotate the navel in the transverse
(horizontal) plane, in one direction and then the
other; then, starting at the base of the spine, do a
vertebra-by-vertebra version of these horizontal
rotations, moving the axis of rotation up one
vertebra at a time. Still in the chair, rotate the
head in both directions.
Spinal flexion and extension can be performed
standing or sitting. On his own, the client will find
it easier to do spinal extension exercises in the
prone position, raising the upper and lower body
separately, then simultaneously, actively (bow or
locust movements) or passively (extending the
arms to passively extend the upper spine). Check
whether the client is a MacKenzie or Williams
type, and let flexion or extension prodominate
accordingly. (Some people with back problems
have normal lordosis; give them equal amounts.)
To create kinesthetic awareness, perform these
exercises very slowly, feeling each vertebra.
On the floor: Roll from side to side on the floor.
On hands and knees, divide the back into four
segmentsㅡlower, waist, middle and upperㅡand
separately raise and lower each segment
repeatedly. (In Mark's first session, this was
followed by massage in the prone position, with
the knees drawn under the abdomen.) In the
supine position, knees bent and apart, soles
touching, groin as open as possible, bring each
knee alternately all the way over to the opposite
side and back again. Hold the breath on the inhale,
raise and lower the abdomen 10 times, then hold
the breath on the exhale and do the same thing.
Next, as you inhale, picture yourself filling with
air like a pitcher filling with water all the way up
to the top of the chest; picture the air pouring out
as you exhale. Make circles with the fingers, then
the wrist, then the forearm, tapping on muscles
(especially flexors) proximal to the joint with the
other hand, to dampen the involvement of
unnecessarily recruited muscles. Rotate the shoulder.
Standing, kick each leg sideways. Stand on a stair
or step, let one leg hang down and rotate it in both
directions. With your back to the stairs, lift each
leg alternately to the lowest stair. Then walk
backward.
Massage therapist Ferrell was advised to follow
up with deep tissue massage to the entire thoracic
area and gentle effleurage*, tapotement and
vibration to the lower and upper back.
* Effleurage as (noun) 1.a form of massage
involving a repeated circular stroking movement
made with the palm of the hand. (verb) 1.massage
with a circular stroking movement."effleurage the
shoulders and press gently"
Donegan practiced the exercises for two
hours a day; as his endurance increased, he
went up to four hours a day and then six.
He enrolled in the School for Self-Healing
and is now an advanced student. Recently
he had surgery to remove the bolts and braces from his back. When he recovered consciousness after the surgery, he began getting massage and doing movement exercisesㅡhead and neck rotationsㅡin the hospital bed. "The massage was a stronger painkiller than three pain pills, and lasted longer," he said. Two and a half weeks later, the swelling had disappeared and he could ride his beloved bike again.
"Now I feel that I've created enough
looseness and awareness in my body so I
know the next stepㅡhow to respect my
pain, not move it, stay in my good range ㅡthen
move it, move through it, soften it,
move more fluidly" he said. "The worst
thing about the pain was haw it isofated
me socially. These days, I can visit my
friends, go there on my bike, hang out,
without having to get up and leave because
the pain is too bad. I have a full social life
and I'm building a massage and movement
business in Ukiah. I feel like in two years
I'll have fully recovered."
Meir Schneider, Ph.D., L.M. T, an internationany
known therapist and educator, is
the creator of the Meir Schneider Self-Healing
Method the author of two books,
Self-Healing My Lie and Vision andThe
Handbook of Self-Healing, and the
founder/director of the Center and School for
Self-Healing in San Francisco. As a teenager,
he overcome blindness caused by congenital
cataracts and other serious vision problems and
today has an unrestricted driver's license.
Carol Gadup is an advanced student of
Self-Healing, Registrar of the School for Self-
Healing, staff writer of the Self-Healing
Research Foundation, and the author of
numerous magazine articles. She studied
physical therapy at the Mayo Clinic and is
now a master's degree candidate in research
psychology at San Francisco State University .

1.⇧On hand and knees, Donegan raises and low the upper back.
Source: http://self-healing.org/wp-content/uploads/2009/01/1moving-out-of-back-problems.pdf
says, "I'm fidgety because of pain; my body's
telling me to move, so I do it everywhere on the
bus, sitting around with friends,wherever I am."
Donegan, 36, is recovering from a very painful
back problem that nearly crippled him, a
herniated inter-vertebral disk in the lumbar
spine. He weaned himself off heavy medications
offered by physicians and chose instead to heal
himself through natural movement, the key
element in self-healing.
Moving in a natural way frees you. It is well-
known in movement science that the skilled
performer has more degrees of freedom
(movement choices) than the novice. When you
look at a film of Fred Astaire and Ginger
Rogers dancing, you feel their looseness, ease
and pleasure in movement. It says a lot about
our culture that they had to work hard to make
it second nature to move easily. As they dance,
you see that their muscles work only as hard as
appropriate and don't substitute for the work of
other muscles (the principle of isolation).
Without tensing up the abdominals, they move
loosely from their center (the navel area). It's
much less effortful, energy-costly and wearing
than the "normal" movement patterns most of us
exhibit, which eventually create chronic health
problems.
Athletes and dancers don't necessarily move
naturally; when they use the body as a tool, they
block out a sense of its problems and needs.
Natural movement comes out of kinesthetic
awareness, a deep, subtle sense of movement-of
breath, energy, blood and other fluids throughout
the body, of joints finding their full range in all
planes, of muscles becoming supple, strong and
balanced. You become aware of the body's
specific need for movement at any given time.
Natural movement healsㅡit increases circulation,
reduces inflammation, creates strength,
endurance and a sense of well-being, and
nurtures every part of the body, including the
joints. Helping the client restore natural
movement is essential in working with joint and
spine problems.
Unfortunately, most people move in an
unbalanced, constricted way. This kind of
movementㅡpatterns of overuse, under-use and
misuseㅡis damaging to the joints, including
those of the spine. Doing more of it in the name
of "exercise" will only make you worse.
We suggest reviewing the article, "Movement is
Life," (Issue #60, March/April 1996); those
exercises and principles are helpful for people
with back problems.
A back problem years in the making
When Donegan was 29, his job required him to
climb up and jump down to fetch items from
grocery stockrooms many times a day. "We were
expected to move fast," he said. He woke up one
morning feeling that his left leg didn't want to
move. A chiropractor diagnosed herniated disk
(also known as disk prolapse or slipped disk), a
complication of degenerative disk disease. Like
cartilage, intervertebral disks in the spinal
column are believed by physicians to degenerate
inevitably, beginning at early adulthood. As a
complication, the disk may herniate or rupture. A
strong ligament keeps it from bulging directly
backward, so it moves posterolaterally, where it
may compress or stretch a spinal nerve root.
Posterolateral: situated on the side and towards
the back of the body. The result is radiating pain,
muscle weakness and sensory losses, always
along the distribution of the spinal nerve. This is
actually one form of sciatica, which can also
begin with compression further down the nerve.
Most prevalent in young men, herniated disk is
rare after middle age, because the disk has lost a
lot of its mass.
Four months of chiropractic treatment only
aggravated the problem. Donegan tried physical
therapy, and it worsened again, until muscle
spasm and pain prevented movement in the leg
altogether.
Two surgeries brought only temporary respite.
In the first operation, part of the disk and of the
bony arch around the spinal cord were trimmed
away; in the second, more of the disk was
removed and two vertebrae were fused together.
After the second surgery, new symptoms came
onㅡnumbness in the left leg, high blood pressure
, irregular heart rate, bowel and bladder
problems. The right leg had been the anchor for
crutch walking; now he lost sensation and
movement in it, too.
"I was looking at a wheelchair next," Donegan
said. "I was depressedㅡmy whole world was
falling apart. The pain gave me nausea and
vomiting. Let me tell you about extreme pain.
You can take it for a day and it's okay. Two days,
and you start getting tired of it, but on the third
day, you don't have anything left. You're not you
anymore."
Another surgeon told Donegan he could remove
the rest of the damaged disk and stabilize the
region with bone transplants and internal braces
and screws. There would be a new source of pain,
however, from the braces. The surgery restored
his ability to walk but left his back swollen and
painful, and "I had nothing left, no will,"Donegan
said. At a pain clinic in Mendocino, California,
Donegan began working with massage therapist
Audrey Ferrell, who practices neuromuscular
therapy. Ferrell gave him massage and movement
exercises. Gradually his pain abated enough that
he could resume his favorite activity, bicycling.
''I gave the doctor back all of his prescription
pain medications; the only thing I kept was over-
the-counter ibuprofen." A year later, Ferrell
brought him to Meir Schneider. " Meir glanced at
me and told me where my pain was," Donegan
recalls.
While Schneider's evaluation seemed fast and
effortless to Donegan, he used, as always, the
method he teaches students: start with
observations of the client walking both forward
and backward, sitting, climbing stairs and doing
other functional tasks. Overall, Schneider says he
assesses stiffness vs. fluidity in the movement of
each body segment; these are issues with many
health problems. The key is isolation, or
independent movement of each body segment.
"In the extreme case," he says, "paralyzed people
have a concept of 'legs' that needs to be
differentiated; they've forgotten that their legs
can move separately from each other. Without
isolation, you have stiffness.
"Often, with back problems like Mark's,"
Schneider says, "the way one has used the legs
throughout life creates lower back damage.
Mark's knees never fully extend as he walks. He
pushes himself from the upper backㅡ there is
too much forward lean. At the time, he held his
head forward and his shoulders forward and up;
this has improved. Bicycling fit right into this
dynamic posture and aggravated it. Mark's back
is poorly organized, with extreme stiffness in the
thoracic paraspinals and weakness,
comparatively, above and below.

⇧Thoracic Paraspinal Muscle Location and Trigger Points
The Thoracic Paraspinal muscles run lengthwise, parallel to the spine. There are actually two layers of muscle that lie one on top of the other. Because these muscles attach to the vertebrae, or bones of the spine, they can cause problems with spinal misalignment and damage to the intervertebral discs.
The pain of Trigger Points in the Thoracic Paraspinal muscles often feels like it originates in the spine itself. The muscles feel hard and rigid, causing stiffness and decreased movement. It often feels as though the entire back is in spasm, which should respond to treatment with heat and superficial massage. When these treatments do not decrease the pain and spasm, Trigger Points are more likely the cause. Extreme tension in these muscles can lead to scoliosis, or a curvature of the spine.
Due to the close proximity of these muscles with the spine and nerves, Trigger Points in these muscles can also refer pain that mimics problems with organs of the chest and abdomen, such as appendicitis, kidney stones, angina, and lung problems.

Thoracic Paraspinal Stretch ⇧
1. Sit in a chair to stabilize hips.
2. Cross arms at mid forearm, and slowly roll forward, until a stretch is felt
3. Hold for 10-15 seconds.
4. Repeat three times, at least three times daily.
"His face and neck hold a lot of unresolved
emotionㅡjaw locked, sternodeidmastoids and
anterior neck generally very tight. His
abdominals are also extremely stiff. His stiff
areas-anterior neck, anterior and posterior chest,
and abdominal dominate his every movement.
"Mark is strong, fast and capableㅡhe's spent
years weightlifting and wrestling. Unfortunately,
being beefed up makes it harder to clear up
movement imbalances; you've invested that
much more in bad movement patterns.
''With movement imbalances, muscles ate
working in packs-big, insensate blocks, where a
group of proximal muscles tense up to 'help'
inappropriately with the work of a distal muscle.
You may see a psoas / pectorals /
stemocleidomastoid/scalene block like Mark's.
Or your client may have a gluteal/hamstring/
paraspinal/shoulder block, coupled with weak
neck and face, a pattern often seen in near-
sightedness. Or you may see an arched lower
back, protruding chest, with overworked upper
trapezius, lower pectorals, rhomboids and
paraspinals; this pattern goes with farsightedness.
Massage therapists need to carefully identify the
client's whole block."
Shortly after the dynamic posture evaluation,
Schneider's massage begins; it is a major
evaluative tool. "I observe the client's breathing
habits, generally and specifically.
People breathe into an area that is being
massaged; areas where this is delayed are
problematic. Mark's breathing was very
shallow, in the chest mostly, with effortful
exhalations. He didn't breathe at all into the
back. And there were, as I expected, arthritic
and fused joints in the lumbar area.
"I saw that Mark's problems started a long time
before he ever had symptoms. Too many people
look at the end resultㅡthe herniated disk in
Mark's case-of a lifelong movement problem as
if this symptom were the real problem you have
to solve, but it's not. Mark learned early on that
he has to fight for survival; it's in every move he
makes (Mark is a survivor of childhood physical
abuse). The problem may have started with
psychological armoring. It wasn't the job-related
jumping that hurt his back: it was the stiffness in
his jumping. As his pain developed, Mark may
have physiologically splinted against it
(tightened up muscles to shore up an area the
body perceives as weak or threatened),
intensifying his muscle spasms or adding more.
To heal himself, Mark was going to have to
change his movement patterns, and this was
going to create changes at every level of his being."
Physical therapy sees essentially two kinds of
muscle imbalances involved in lower back pain
ㅡtoo much lumbar curve (hyperlordotic) or too
little (flat lower back). They may apply the
classic testㅡhave the patient stand against a
wall and see how many hands' widths he or she
can fit into the lumbar curve-one is normal,
zero or two are problematic. The patient is
then asked to do a standing forward bend and
backbend and describe how each changes the
pain. If it lessens or radiates less, this is the
therapeutic direction for movementㅡpain in the
flat lower back is relieved by backbending; in the
hyperiordotic lower back, by forward bending.
Two leaders in the rehabilitation of backs have
lent their names to these diagnoses/regimen the
Williams protocol is predominantly a spinal
flexion program for hyperlordotic backs; the
MacKenzie, spinal extension for flat low backs.
Schneider says this is useful, as fir as it goes.
Carol Gallup thinks the Williams MacKenzie
distinction is often under-emphasized in the
holistic health community. "A few years ago,
during physical therapy school, I worked briefly
with a young woman with serious lower back
pain, radiating down the legs, with movement
and sensory losses in the legs. Kendra's back
pain began after she allowed a friend who
happened to be a holistic health practitioner to
work with her for a few months to 'correct' her
posture; before that she had had no problem.
This practitioner believed, on the basis of his
training, that the normal lumbar curve was
unhealthy, and that every lower back should be
flat. He did indeed flatten out her lumbar curve
ㅡand created a serious back problem for his
client.
"I see two morals in this story-first, the old
saying, 'if it ain't broke, don't fix it.' Second,
listen to the bioengineers and biomechanics.
They're telling us that the incredible ability of
the back to withstand the stresses we subject it
to every day is caused in part by its shape-
essentially, it's a spring, with the resiliency of a
spring, and it needs the normal amount of
kyphosis* in the upper back and the normal
amount of lordosis in the lower back.
[*Kyphosis (from Greek κυφός kyphos, a hump) is an abnormally excessive convex kyphotic curvature of the spine as it occurs in the cervical, thoracic and sacral regions. (Abnormal inward concave lordotic curving of the cervical and lumbar regions of the spine is called lordosis.)
Hunchback / Kyphosis⇧]
*
⇧ *Lordosis is defined as an excessive inward curve of the spine. It differs from the spine's normal curves at the cervical, thoracic, and lumbar regions, which are, to a degree, either kyphotic (near the neck) or lordotic (closer to the low back).]

So when I met Kendra she had a 'MacKenzie'
back. I gave Kendra some standing and other
[types of] backbends, and her pain immediately
started to lessen and centralize (radiate less), a
sure sign that backbending was an important
direction to take with her therapy.
"I myself happen to tend in the opposite
direction, hyperlordoticㅡa 'Williams' back. I've
found that I do best if, for every six or eight
spinal flexion exercises, I do two or three spinal
extensions. Bear in mind also that serious lower
back pain can occur gram for clients with spine,
joint and when the lower back curve is normal
ㅡthe client may still have muscle tightness,
muscle spasm, very limited mobility."
With the Williams protocol, physical therapists tend to automatically add exercises to strengthen
the abdominals. We know someone who had such severe back pain
that he was admitted to the hospital; a physical therapist looked at his chart and said, "You'll have to strengthen those abdominals; you've got a muscle imbalance causing all that pain." To prove her point, she casually poked at his abdomenㅡand then looked shocked. The patient was a rugby player with magnificent abdominals. He was indeed hyperlordotic, but those strong abdominals weren't correcting it.
Why not? Schneider feels that the problem in
unbalanced movement patterns lies with the
nervous system predominantly and the muscles
only secondarily. Thus, strengthening the
underused muscles alone or in conjunction with
spinal flexion or extension exercises will not
correct the problem. "The brain ignores muscles
in areas it regards as unsupported," he explains.
"'Support' is good mobility in the muscles, not
brute strength; Mark, for example, is very strong
but stiff in the thoracic back, and his brain registers
this as nonsupport and tends to ignore muscles
above it." Schneider's view is at odds with that of
chiropractors and physical therapists, who routinely
make use of lumbar belts, believing they support
the lower back by immobilizing it.
"Hyperflexibility is also seen by the brain as nonsupport-if your client is pathologically loose-jointed, congenitally or from bad stretching programs, there's compensatory muscle tightness."
We need to interfere with the neural habit of
overusing some muscle groups, as if they are the
only muscles it is natural to work, and ignoring
others. A good program for clients with spine,
joint and many other problems involves serious reprogramming. Most of us have immobile toes, for example, from walking in shoes on cement sidewalks, so that our toes and feet didn't develop a pattern of pleasurable sensorimotor interaction with the ground; we can create such a pattern by walking and running on a beach or grassy surface. This is importantㅡstiff feet and calves contribute stiffness to every other joint in the body. And we can interfere with other rigidities in our walk by walking and running backwards. Coordination exercises are very helpful. We can explore the full range of motion of our joints, with movements that take us through many planes (we tend to live in the sagittal, or forward/backward, plane). Massage is essential, since it breaks adhesions and creates new sensory input to the brain, sending it the message that muscles can be soft and mobile. And it is essential for clearing up muscle spasms. Rolling on the floor or the ground is especially helpful, recruiting side muscles that are usually ignored.
We've used the general terms "stiffness", "fluidity,"
and "immobility" purposely when talking about
evaluating movement; these are fairly easy
distinctions to make, visually and through touch.
Later, the evaluator can note muscle spasms or
limited range of motion at the joint. Schneider
found limited joint mobility in Donegan's lumbar
spine and habitual muscle spasm in his psoas,
pectorals, serratus anterior, intercostals, scalenes
and sternocleidomastoid.
"More natural ways of moving-muscles doing only their own work, not adding unnecessary effort, what we call isolationㅡcan't fully take hold until habitual muscle spasm is gone. And it goes away slowly, very slowly, over time. You can clear it up in the sessionㅡwith Self-Healing Neurological Massage (a light-pressure, very vigorous vibrating touch that is a cross between brisk shaking of the muscle and tapotement), tapotement, deep tissue massage, breathing exercisesㅡand the client
walks out much looser, feeling great, thinking
you're wonderful. But the dynamic posture and
the lack of awareness that put it there didn't go away. The client will go home and torque or overload or suddenly strain the back, and the pain may return in full force, and unless you've educated them about the process, they may think the session was a failure. You need to loosen them up and get them doing the movement exercises that teach the brain how to isolate, how to move naturally. There's a long transition period with ups and downs as the new adaptations start, and then eventually they're complete and the spasm is gone."
Donegan was already on a one-hour daily exercise regimen of exercycle workouts, standing lateral and forward bends, knee bends, and stretches for the groin, hamstrings, and calvesㅡ"the standard ones for back pain, on printed sheets that you get from the physical therapist and the chiropractor," Donegan recalls. "They were teaching me movements, trying to figure out bow to get my legs going again, and it wasn't helping. Meir taught me how to move. He pointed out places I was
holding myself; I had an immediate knowledge
that the movements he gave me would release
that area and that release there was the key.
Every exercise improved a symptom."
The regimen that Schneider gave Donegan is described below because it is helpful with his pattern of stiffness and muscle tension, and above all, because it is helping him develop kinesthetic awareness so that he can sense for himself the movements that his body needs. No one program is universally helpful; this one should be looked at in the light of the principles we have discussed.
Exercises to reprogram for soft, fluid movement
The exercises need to be repeated many times; the
effect on the nervous system is slow and
cumulative. All rotations should be done in both
directions.
Seated: First, rotate the navel in the transverse
(horizontal) plane, in one direction and then the
other; then, starting at the base of the spine, do a
vertebra-by-vertebra version of these horizontal
rotations, moving the axis of rotation up one
vertebra at a time. Still in the chair, rotate the
head in both directions.
Spinal flexion and extension can be performed
standing or sitting. On his own, the client will find
it easier to do spinal extension exercises in the
prone position, raising the upper and lower body
separately, then simultaneously, actively (bow or
locust movements) or passively (extending the
arms to passively extend the upper spine). Check
whether the client is a MacKenzie or Williams
type, and let flexion or extension prodominate
accordingly. (Some people with back problems
have normal lordosis; give them equal amounts.)
To create kinesthetic awareness, perform these
exercises very slowly, feeling each vertebra.
On the floor: Roll from side to side on the floor.
On hands and knees, divide the back into four
segmentsㅡlower, waist, middle and upperㅡand
separately raise and lower each segment
repeatedly. (In Mark's first session, this was
followed by massage in the prone position, with
the knees drawn under the abdomen.) In the
supine position, knees bent and apart, soles
touching, groin as open as possible, bring each
knee alternately all the way over to the opposite
side and back again. Hold the breath on the inhale,
raise and lower the abdomen 10 times, then hold
the breath on the exhale and do the same thing.
Next, as you inhale, picture yourself filling with
air like a pitcher filling with water all the way up
to the top of the chest; picture the air pouring out
as you exhale. Make circles with the fingers, then
the wrist, then the forearm, tapping on muscles
(especially flexors) proximal to the joint with the
other hand, to dampen the involvement of
unnecessarily recruited muscles. Rotate the shoulder.
Standing, kick each leg sideways. Stand on a stair
or step, let one leg hang down and rotate it in both
directions. With your back to the stairs, lift each
leg alternately to the lowest stair. Then walk
backward.
Massage therapist Ferrell was advised to follow
up with deep tissue massage to the entire thoracic
area and gentle effleurage*, tapotement and
vibration to the lower and upper back.
* Effleurage as (noun) 1.a form of massage
involving a repeated circular stroking movement
made with the palm of the hand. (verb) 1.massage
with a circular stroking movement."effleurage the
shoulders and press gently"
Donegan practiced the exercises for two
hours a day; as his endurance increased, he
went up to four hours a day and then six.
He enrolled in the School for Self-Healing
and is now an advanced student. Recently
he had surgery to remove the bolts and braces from his back. When he recovered consciousness after the surgery, he began getting massage and doing movement exercisesㅡhead and neck rotationsㅡin the hospital bed. "The massage was a stronger painkiller than three pain pills, and lasted longer," he said. Two and a half weeks later, the swelling had disappeared and he could ride his beloved bike again.
"Now I feel that I've created enough
looseness and awareness in my body so I
know the next stepㅡhow to respect my
pain, not move it, stay in my good range ㅡthen
move it, move through it, soften it,
move more fluidly" he said. "The worst
thing about the pain was haw it isofated
me socially. These days, I can visit my
friends, go there on my bike, hang out,
without having to get up and leave because
the pain is too bad. I have a full social life
and I'm building a massage and movement
business in Ukiah. I feel like in two years
I'll have fully recovered."
Meir Schneider, Ph.D., L.M. T, an internationany
known therapist and educator, is
the creator of the Meir Schneider Self-Healing
Method the author of two books,
Self-Healing My Lie and Vision andThe
Handbook of Self-Healing, and the
founder/director of the Center and School for
Self-Healing in San Francisco. As a teenager,
he overcome blindness caused by congenital
cataracts and other serious vision problems and
today has an unrestricted driver's license.
Carol Gadup is an advanced student of
Self-Healing, Registrar of the School for Self-
Healing, staff writer of the Self-Healing
Research Foundation, and the author of
numerous magazine articles. She studied
physical therapy at the Mayo Clinic and is
now a master's degree candidate in research
psychology at San Francisco State University .
1.⇧On hand and knees, Donegan raises and low the upper back.
Source: http://self-healing.org/wp-content/uploads/2009/01/1moving-out-of-back-problems.pdf

No comments:
Post a Comment