Chapter 7.
The fundamental fuel for your body is glucose, a simple sugar that provides all your cells with he energy they need to function, heal, grow, and thrive.
Glucose keeps us goingㅡand keeps us alive. The central nervous system runs on glucose, as does every organ in the human body, including the heart. Glucose is what we use to build and sustain muscle, and it performs vital functions such as repairing damaged tissue and cells.
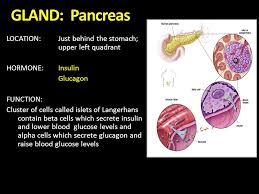
When you eat food, your body breaks it down into glucose and places it in your bloodstream so it can travel too all your cells. However, your cells can't access the glucose directly. They need some help from your pancreas, which is a large endocrine gland located behind your stomach.

(Click here to view more on Human Anatomy Study)

Your pancreas is constantly monitoring your blood stream. When it detects a rise in glucose levels, it responds by producing a hormone called insulin. Insulin attaches to your cells and signals them to open up and absorb the glucose from your blood. Insulin therefore both allows your cells to get the energy they need and ensures your blood glucose levels remain stable.
If your bloodstream has more glucose than your cells can consume ㅡ for example, if you've eaten a particularly heavy meal ( maybe animal ribs slathered in syrupy barbecue sauce; in other words, a lot of fat combined with sugar) ㅡ your insulin directs the extra glucose to be stored in your liver. At some later point when your glucose levels run low ㅡ for example, in between meals, or during periods of intense physical activity ㅡ your liver will release stored glucose for use by your cells. That is, if your liver is strong and functions well.
This is normally an effective system for optimal glucose use. However, it starts to go wrong if your pancreas fails to produce enough insulin when it's needed. It also goes wrong if some of your cells start refusing to let the insulin attach and open the cells up to receive glucose; this is called insulin resistance.

When either or both of these problems occur, not enough glucose is removed from your blood by your cells. Your body will expel some of the excess glucose in your urine, (ants will be attracted to your urine) which may cause you to urinate more frequently, and also dehydrate you and make you feel thirsty.
If your pancreas is not creating enough insulin when your body needs it. and/or if you're experiencing insulin resistance, and if these issues lead to exceptionally high blood glucose levels, you're at risk for type-2 diabetes. Around 35 million people (2014 figure) have this disease in the U.S.A alone. And another 95 million have prediabetes, with blood glucose levels higher than normal but not yet at diabetes levels.

•The Fasting Plasma Glucose (FPG) test is performed after a person has fasted for at least 8 hours. A sample of blood is taken from a vein in the arm. If the blood glucose level is greater than or equal to 126 mg/dl, the person is retested and, if the results are consistent, diagnosed with diabetes.
•The Glucose Tolerance Test (GTT), also referred to as the Oral Glucose Tolerance Test (OGTT), is a method which can help to diagnose instances of diabetes mellitus or insulin resistance.
The test is a more substantial indicator of diabetes than finger prick testing.
What is an OGT test?
The test is used to determine whether the body has difficulty metabolising intake of sugar/carbohydrate.
The patient is asked to take a glucose drink and their blood glucose level is measured before and at intervals after the sugary drink is taken.
Why is an oral glucose tolerance test done?
This can be a useful test in helping to diagnose:
🔵 Pre-diabetes
🔵Gestational diabetes in pregnant women
🔵Insulin resistance
🔵Reactive hypoglycemia
How is the test performed?
Before the test you will be asked not to eat, or drink certain fluids, for up to 8 to 12 hours before the test.
You may be asked to not take certain medications in the lead up to the test, but only if these would affect the test results.
For the test itself, you will first have blood taken to measure your blood glucose level before the test. The next stage is to take a very sweet tasting, glucose drink.
Further blood samples will then be taken either at regular intervals of say 30 or 60 minutes or a single test after 2 hours. The test could take up to 3 hours.
Between blood tests you will need to wait so it’s best to have some reading material, or something else to keep you occupied, with you.
What should the OGTT results be?
People without diabetes:
🔵Fasting value (before test): under 6 mmol/L
🔵At 2 hours: under 7.8 mmol/L
People with impaired glucose tolerance (IGT):
🔵Fasting value (before test): 6.0 to 7.0 mmol/L
🔵At 2 hours: 7.9 to 11.0 mmol/L
Diabetic levels:
🔵Fasting value (before test): over 7.0 mmol/L
🔵At 2 hours: over 11.0 mmol/L



The fundamental fuel for your body is glucose, a simple sugar that provides all your cells with he energy they need to function, heal, grow, and thrive.
Glucose keeps us goingㅡand keeps us alive. The central nervous system runs on glucose, as does every organ in the human body, including the heart. Glucose is what we use to build and sustain muscle, and it performs vital functions such as repairing damaged tissue and cells.
When you eat food, your body breaks it down into glucose and places it in your bloodstream so it can travel too all your cells. However, your cells can't access the glucose directly. They need some help from your pancreas, which is a large endocrine gland located behind your stomach.

(Click here to view more on Human Anatomy Study)

Your pancreas is constantly monitoring your blood stream. When it detects a rise in glucose levels, it responds by producing a hormone called insulin. Insulin attaches to your cells and signals them to open up and absorb the glucose from your blood. Insulin therefore both allows your cells to get the energy they need and ensures your blood glucose levels remain stable.
If your bloodstream has more glucose than your cells can consume ㅡ for example, if you've eaten a particularly heavy meal ( maybe animal ribs slathered in syrupy barbecue sauce; in other words, a lot of fat combined with sugar) ㅡ your insulin directs the extra glucose to be stored in your liver. At some later point when your glucose levels run low ㅡ for example, in between meals, or during periods of intense physical activity ㅡ your liver will release stored glucose for use by your cells. That is, if your liver is strong and functions well.
This is normally an effective system for optimal glucose use. However, it starts to go wrong if your pancreas fails to produce enough insulin when it's needed. It also goes wrong if some of your cells start refusing to let the insulin attach and open the cells up to receive glucose; this is called insulin resistance.

When either or both of these problems occur, not enough glucose is removed from your blood by your cells. Your body will expel some of the excess glucose in your urine, (ants will be attracted to your urine) which may cause you to urinate more frequently, and also dehydrate you and make you feel thirsty.
If your pancreas is not creating enough insulin when your body needs it. and/or if you're experiencing insulin resistance, and if these issues lead to exceptionally high blood glucose levels, you're at risk for type-2 diabetes. Around 35 million people (2014 figure) have this disease in the U.S.A alone. And another 95 million have prediabetes, with blood glucose levels higher than normal but not yet at diabetes levels.
•The Fasting Plasma Glucose (FPG) test is performed after a person has fasted for at least 8 hours. A sample of blood is taken from a vein in the arm. If the blood glucose level is greater than or equal to 126 mg/dl, the person is retested and, if the results are consistent, diagnosed with diabetes.
•The Glucose Tolerance Test (GTT), also referred to as the Oral Glucose Tolerance Test (OGTT), is a method which can help to diagnose instances of diabetes mellitus or insulin resistance.
The test is a more substantial indicator of diabetes than finger prick testing.
What is an OGT test?
The test is used to determine whether the body has difficulty metabolising intake of sugar/carbohydrate.
The patient is asked to take a glucose drink and their blood glucose level is measured before and at intervals after the sugary drink is taken.
Why is an oral glucose tolerance test done?
This can be a useful test in helping to diagnose:
🔵 Pre-diabetes
🔵Gestational diabetes in pregnant women
🔵Insulin resistance
🔵Reactive hypoglycemia
How is the test performed?
Before the test you will be asked not to eat, or drink certain fluids, for up to 8 to 12 hours before the test.
You may be asked to not take certain medications in the lead up to the test, but only if these would affect the test results.
For the test itself, you will first have blood taken to measure your blood glucose level before the test. The next stage is to take a very sweet tasting, glucose drink.
Further blood samples will then be taken either at regular intervals of say 30 or 60 minutes or a single test after 2 hours. The test could take up to 3 hours.
Between blood tests you will need to wait so it’s best to have some reading material, or something else to keep you occupied, with you.
What should the OGTT results be?
People without diabetes:
🔵Fasting value (before test): under 6 mmol/L
🔵At 2 hours: under 7.8 mmol/L
People with impaired glucose tolerance (IGT):
🔵Fasting value (before test): 6.0 to 7.0 mmol/L
🔵At 2 hours: 7.9 to 11.0 mmol/L
Diabetic levels:
🔵Fasting value (before test): over 7.0 mmol/L
🔵At 2 hours: over 11.0 mmol/L
• Hemoglobin A1c, often abbreviated HBA1C, is a form of hemoglobin (a blood pigment that carries oxygen) that is bound to glucose. The blood test for HbA1c level is routinely performed in people with type 1 and type 2 diabetes mellitus. Blood HbA1c levels are reflective of how well diabetes is controlled.
As many as 35 percent of those with prediabetes will develop type-2 diabetes within six years.
Medical professionals do not know why type-2 diabetes happens. This is evident in the diets that physicians and dieticians recommend to diabetics; if they knew what was really happening in these patients' bodies, they'd offer completely different food advice. While doctors get some elements of treatment right, they are not able to offer an understanding of how or why this disease starts.
Here I will tell you precisely what cause type-2 diabetes. I will also truly explain how insulin resistance occurs, as well as what hypoglycemia is and how to get your system back in balance enough so your body can have the chance to heal.
TYPE-2 DIABETES SYMPTOMS
If you have type-2 diabetes, you may experience one or more of the following symptoms. Note that it's possible to be in the early stages of diabetes and not experience any symptoms.
• Unusual thirst, dry mouth, frequent urination: this is because your body is using up water to expel excess glucose via your urine.
• Blurry vision: as you become dehydrated, your body may pull water from the lenses of your eyes to help flush out the excess glucose.
• Unusual hunger: this is because your cells are not getting all the glucose they need to feed themselves.
• Fatigue and irritability: as you're not getting the energy you normally do when your cells are fully fueled with glucose.
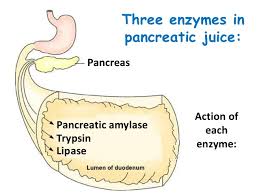
• Digestive problems: your pancreas does not just make insulin; the pancreas make enzymes to help your body break down foods. If your pancreas is under-performing, this creates not only an insulin deficiency but also an enzyme deficiency, making it harder for your body to digest anything.
• Hypoglycemia: these energy lows ㅡ blood sugar drops that occur as often as every other hour ㅡ are the result of weakness of the liver and under-active adrenals.
WHAT REALLY CAUSES TYPE-2 DIABETES AND HYPOGLYCEMIA
While medical communities are unaware of this, the causes of both type-2 diabetes and hypoglycemia typically begin with the adrenal glands.
The adrenal glands (also known as suprarenal glands) are endocrine glands that produce a variety of hormones including adrenaline and the steroids aldosterone and cortisol. They are found above the kidneys. Each gland has an outer cortex which produces steroid hormones and an inner medulla.
When you are up against continual stress and experiencing difficult and unavoidable trials in life, it sets your adrenal glands to flood your body with adrenaline, a hormone that charges you with emergency energy. While this is a helpful response for dire straits, if you're continually operating in crisis mode and are not able to physically burn off the corrosive adrenaline saturating the tissues of your organs and glands, the adrenaline can eventually do serious damage.
Your pancreas is normally as smooth as a baby's bottom. But chronic scorching by fear-based or other negative-emotion-based adrenaline will wear away at the pancreas, creating calluses that turn the pancreas thick and hard.

It's like this: When you're born, your pancreas is like a brand-new credit card. Some come into the world with a sweet deal ㅡ a high spending limit, a generous cash credit line, and a cache of frequent flyer miles just for signing up. Others come into the world with lower credit limits, higher interest rates, and fewer bonuses. Either way, you can use that thing up if you're not careful. When people go through life wearing themselves down and taming the stress with fried of high-fat foods, ice cream, cookies ... they run up the balance on the pancreas and use up those frequent flyer miles.
Over time, this damages the pancreas's ability to produce enough insulin to remove all the glucose it should from your bloodstream. And this under-performance alone is enough to create type-2 diabetes.
That's not the end of it. Your entire body is damaged by chronic floods of negative-emotion-based adrenaline. Especially if you eat when you're emotional, your pancreas will produce insulin that mixes with the adrenaline in your bloodstream, leading your body to associate the insulin with the fear-based adrenaline that's hurting it. Over time, this can make many of your cells "allergic" to your adrenaline/insulin blend and cause them to shun both hormones. Medical research has not yet uncovered this "Franken-sulin" hybrid ( as I call it), nor has it understood that the physical body revolts in this way. It's one of the primary causes of pancreatic weakness, which leads to lowered insulin production and nonacceptance of glucose in the body's cells.
Heavy, rich meals can trigger excess adrenaline production, too.That's because the adrenals are like a fire station, and fat triggers the alarm bell. When the adrenals get the signal that high levels of fat are in the bloodstreamㅡand therefore have the potential to put the pancreas and liver in immediate dangerㅡthe firehouse (the adrenals) sends out the fire trucks (adrenaline) to address the situation. That rush of adrenaline increase digestive strength to help move the fat through your system and protect you, but you pay a price, as this process can weaken the pancreas over time.
On the flip side, your adrenal glands may be under-performingㅡthat is, producing too little adrenaline. This makes your pancreas work overtime to try to compensate. If this condition is chronic, your pancreas will become inflamed or enlarged, and may eventually start under-performing as well.
Then again, you can have adrenal fatigue, in which your unstable adrenals are sometimes producing too little adrenaline and sometimes producing way too much. This can batter your pancreas as it becomes inflamed to compensate for dry spells of adrenaline and then gets scorched by floods of it.
Once your pancreas becomes dysfunctional, it can suffer damage from itself. That's because in addition to insulin, your pancreas produces enzymes that aid with digestion. Your pancreas also makes inhibitors that prevent these powerful enzymes from turning on itself as if it were a food to be dissolved. But if your pancreas grows sufficiently defective, it'll start under-producing its inhibitors, at which point the enzymes it produces will create even more damage. On top of that, you'll start experiencing digestive problems .....
A precursor to type-2 diabetes is a fluctuating but low glucose levelㅡcalled hypoglycemiaㅡwhich indicates a major issue with your body's ability to manage glucose properly. This can occur if your liver becomes impaired in its ability to store and release glucose. It can also happen if you're failing to eat at least a light, balanced snackㅡe.g., a fruit (for sugar and potassium) and a vegetable (for sodium)ㅡevery two hours. Regularly skipping meals forces your body to use up the liver's precious glucose storage, driving the body to run on adrenaline; and as previously mentioned, this can damage your pancreas, create insulin resistance, and lead to adrenal fatigue and weight gain over time.
One other major factor is the type of food you eat. There's a common misconception that diabetes is caused by eating a lot of foods with sugar in them. However, it's not actually the sugar that's the problem. It's sugar and fat combinedㅡmainly fat. For example, you could eat fruit all day and every day for the rest of your life and never get diabetes. In fact, eating a lot of fruit is the most effective way to add years to your life, as explained in Chapter 20, "Fruit Fear."
The problem is fat. Most people who consume processed foods and junk foods such as cakes, cookies, doughnuts, ice cream, and so onㅡor people who have a seemingly healthy main dish like chicken but follow it up with dessertㅡtypically eat a lot of fat and a lot of sugar at the same time. While sugar that's not attached to nutrients (e.g.,that isn't coming from fruit or vegetables) is definitely unhealthy, it's the fat that strains your liver and pancreas.
The first thing that will happen is that instant insulin resistance from the high levels of blood fat that result from an animal protein mealㅡwhether lean versions of pork, steak, or chicken, or fast food battered and fried in oilㅡwill stop the body's ability to allow the insulin produced by your pancreas to drive sugar into your cells. This will mean there's a whole lot of sugar floating around the bloodstream that can't go anywhere. A strong liver will help gather up as much glucose as it can to store for a rainy day. Over time, a diet high in animal fat, protein, and processed oils can burden the liver, though. Your liver can reach a vulnerable state from the constant responsibility to clean up the excess glucose in the bloodstream, and from waiting too many hours between meals to be refueled. When the liver becomes overburdened in this way, it dumps all of its glucose storage back into the bloodstream. This can prompt the birthing stage of hypoglycemia.
Since your liver has to take the burden of processing the fat you eat, a diet high in animal fat, which hides in even the lean animal protein people tend to think of as healthy, can make the organ sluggish and unable to store and release glucose the way it should. Large, heavy meals plus glucose dry spells caused by not eating in between can eventually result in type-2 diabetes.
At the same time, your pancreas has to produce enzymes to break down the fat so you can digest it. A lot of fat makes your pancreas work extra hard; and if you've already got other factors straining your pancreas, such as severe negative emotions and/or adrenal glands flooding it with corrosive adrenaline, a diet high in fat may be all that's needed to push your pancreas over the edge and create type-2 diabetes.
The good news is that all the damage described above is absolutely reversible. Next we'll cover how to heal your pancreas, your liver, and your insulin-traumatized cells so you can bring your hypoglycemia or type-2 diabetes to an end.
ADDRESSING TYPE-2 DIABETES AND HYPOGLYCEMIA
Since medical communities don't know the real story of what causes type-2 diabetes and hypoglycemia, they don't provide the proper diet guidance. Typically, they recommend a diet with little to no sugar in it, advising patients to avoid fruit altogether and focus on eating animal protein and vegetables.
Heeding this advice will probably keep you diabetic foreverㅡand not just diabetic and functional, but diabetic and ailingㅡ since the fat in meat is only going to make your condition worse, while eating fruit is critical for healing diabetes. It's imperative to understand that animal fats are what weakened the pancreas and liver to begin with.
Sugar was just the messenger. And in this case, health professionals shoot the messenger. That sugar was showcasing the insulin resistance that had cropped up from a pancreas overburdened by fat.
It's easy to eat a diet high in animal fat without realizingit. Even a lean-cut four-ounce piece of meat will contain a tablespoon of concentrated fat that can burden the pancreas and liver. So when a person is insulin resistant (even from a diet that seems traditionally "healthy") and puts sugar into her or his system, that sugar is going to prompt insulin problemsㅡand suddenly sugar is going to get all the attention, when it's NOT the real instigator.
Think of it like the teenager who throws a party when her parents are out of town. Say her younger brother drinks some punch-drink he didn't realize was spiked, gets sick, and calls Mum and Dad. Then say when they return home to a trashed house and drunk visitors, the big sister (fat) tries to blame the whole thing on her little brother (sugar). But he (sugar) didn't do anything wrong!
Now of course white table sugar and many other sweeteners aren't good for youㅡI'm not recommending you, eat these. Yet to address type-2 diabetes and hypoglycemia, it is critical to lower fat consumption and increase fresh fruit and vegetable consumption. I recommend the cleanse in Chapter 21 : The 28-Day Healing Cleanse to help heal the liver, pancreas, and adrenal glands and stabilize blood sugar levels.
Your doctor may prescribe insulin. While insulin lowers your blood glucose level, it does nothing to address core problems such as damaged adrenal glands, a damaged pancreas, a dysfunctional liver, chronic negative emotions, and/or insulin resistance.
What follows is a more targeted daily approach that focuses on healing every likely cause of your type-2 diabetes or hypoglycemia. You'll also find guidance in Part IV,"How to Finally Heal." How long you'll need to stick with this program depends on how much damage has to be undone. You should notice improvements within a few months, and the complete process typically requires six months to two-and-a-half years.
Bolster Your Adrenal Glands.

The fact that you have type-2 diabetes means it's likely you have an issue with your adrenal glands. Therefore, one step toward healing is to read Chapter 8, "Adrenal Fatigue." You can follow its advice to make your adrenal glands stable and strong.
Healing Foods
Wild blueberries, spinach, celery, papayas,sprouts, kale, raspberries, and asparagus are top foods to eat if you have type-2 diabetes or hypoglycemia. These perform functions such as detoxing the liver, strengthening glucose levels, supporting the pancreas, boosting the adrenal glands and stabilizing insulin.
Take care to avoid certain foods as well, most specifically cheese, milk, cream,butter, eggs, processed oils, and all sugars except raw honey and fruit.
Healing Herbs and Supplements
• Zinc: supports the pancreas and adrenal glands and helps stabilize glucose levels in the blood.
• Chromium: sustains the pancreas and adrenal glands and helps stabilze insulin levels.
• Spirulina (preferably from Hawaii): helps stabilize glucose levels in the blood and aids theadrenal glands.
• Ester-C: this form of vitamin C soothes and bolsters the adrenal glands.
• ALA (alpha lipoic acid): boosts the liver's ability to store and release glucose.
• Silica: helps stabilize the pancreas's release of insulin.
• Purslane: strengthens the pancreas and its production of digestive enzymes.

Health Benefits of Purslane. This wonderful green leafy vegetable is very low in calories (just 16 kcal/100g) and fats; nonetheless, it is rich in dietary fiber, vitamins, and minerals. Fresh leaves contain surprisingly more omega-3 fatty acids (α-linolenic acid) than any other leafy vegetable plant.
Purslane (Portulaca oleracea) or also known as cat's tongue provides many health benefits. It is good for our skin, urinary and digestive systems. It also has a perfect combination between antioxidants, omega 3 fatty acids, potassium, calcium, magnesium and carotene.
• Eleuthero (aka Siberian ginseng): enhances the body's ability to react and adapt, which helps prevent the adrenal glands from overreacting to fear, stress, and other intense emotions.
• Panax ginseng: also enhances the body's ability to react and adapt, which in turn helps prevent the adrenal glands from overreacting to fear, stress, and other intense emotions.
• EPA & DHA (eicosapentaenoic acid and docosahexaenoic acid): helps heal insulin resistance. be sure to buy a plant-based (not fish-based) version.
• Biotin: helps stabilize glucose levels in the blood and supports the central nervous system.
• B-complex: sustains the central nervous system.
• Gymnema sylvestre: helps lower glucose levels in the blood and stabilize insulin levels.

↑Gymnema is a woody climbing shrub native to India and Africa. The leaves are used to make medicine. Gymnema has a long history of use in India's Ayurvedic medicine. The Hindi name, gurmar, means "destroyer of sugar." Today, gymnema is used for diabetes, metabolic syndrome, weight loss, and cough.
• Magnesium: soothes digestive issues caused by an underperforming pancreas. Also calms stressed adrenal glands.
• Vitamin D3 : bolsters the pancreas and adrenal glands, and reduces inflammation. Vitamin D3 (cholecalciferol) is an essential vitamin that can be taken as a supplement to improve overall health or used for treating osteoporosis.
Vitamin D is sometimes called the “sunshine vitamin” because it’s produced in your skin in response to sunlight. It’s a fat-soluble vitamin in a family of compounds that includes vitamins D-1, D-2, and D-3.
Your body produces vitamin D naturally when it’s directly exposed to sunlight. You can also get it through certain foods and supplements to ensure adequate levels of the vitamin in your blood.
Vitamin D has several important functions. Perhaps the most vital are regulating the absorption of calcium and phosphorus, and facilitating normal immune system function. Getting a sufficient amount of vitamin D is important for normal growth and development of bones and teeth, as well as improved resistance against certain diseases.
If your body doesn’t get enough vitamin D, you’re at risk of developing bone abnormalities such as soft bones (osteomalacia) or fragile bones (osteoporosis).
Here are three more surprising benefits of vitamin D.
FIGHTS DISEASE
1. Vitamin D fights disease
In addition to its primary benefits, research suggests that vitamin D may also play a role in:
•reducing your risk of multiple sclerosis, according to a 2006 study published in the Journal of the American Medical Association
•decreasing your chance of developing heart disease, according to 2008 findings published in Circulation
•helping to reduce your likelihood of developing the flu, according to 2010 research published in the American Journal of Clinical Nutrition
REDUCES DEPRESSION
2. Vitamin D reduces depression
Research has shown that vitamin D might play an important role in regulating mood and warding off depression. In one study, scientists found that people with depression who received vitamin D supplements noticed an improvement in their symptoms.
In another study of people with fibromyalgia, researchers found vitamin D deficiency was more common in those who were also experiencing anxiety and depression.
BOOSTS WEIGHT LOSS
3. Vitamin D boosts weight loss
Consider adding vitamin D supplements to your diet if you’re trying to lose weight or prevent heart disease.
In one study, people taking a daily calcium and vitamin D supplement were able to lose more weight than subjects taking a placebo supplement. The scientists said the extra calcium and vitamin D had an appetite-suppressing effect.
In another study, overweight people who took a daily vitamin D supplement improved their heart disease risk markers.
VITAMIN D DEFICIENCY
Beware of D-ficiency
Many factors can affect your ability to get sufficient amounts of vitamin D through the sun alone. These factors include:
•Being in an area with high pollution
•Using sunscreen
•Spending more time indoors
•Living in big cities where buildings block sunlight
•Having darker skin. (The higher the levels of melanin, the less vitamin D the skin can absorb.)
These factors contribute to vitamin D deficiency in an increasing number of people. That’s why it’s important to get some of your vitamin D from sources besides sunlight.
The symptoms of a vitamin D deficiency in adults include:
•tiredness, aches and pains, and a general sense of not feeling well
•severe bone or muscle pain or weakness that may cause difficulty climbing stairs or getting up from the floor or a low chair, or cause you to walk with a waddling gait
•stress fractures, especially in your legs, pelvis, and hips
Doctors can diagnose a vitamin D deficiency by performing a simple blood test. If you have a deficiency, your doctor may order X-rays to check the strength of your bones.
If you’re diagnosed with a vitamin D deficiency, your doctor will likely recommend you take daily vitamin D supplements. If you have a severe deficiency, they may instead recommend high-dose vitamin D tablets or liquids. You should also make sure to get vitamin D through sunlight and the foods you eat.
Food sources of vitamin D
Few foods contain vitamin D naturally. Because of this, some foods are fortified. This means that vitamin D has been added. Foods that contain vitamin D include:
•salmon
•sardines
•egg yolk
•shrimp
•milk (fortified)
•cereal (fortified)
•yogurt (fortified)
•orange juice (fortified)
CASE HISTORY:
Getting a New Perspective on Sugar
Starting in her teens, Morgan battled what she called emotional highs and lows. Her mother, Kim, learned that if Morgan went too long without eating, she'd start to act out with a burst of frustration or fall into tears out of nowhere.
Kim repeatedly took Morgan to the family doctor to have her blood sugar levels evaluated, but Morgan's A1C and other tests would always come back normal. The doctor passed off Morgan's inconsistent behaviour as an aspect of being a sensitiveㅡor maybe even bipolarㅡgirl.
When Morgan was in her early 20s, Kim found an alternative doctor who said Morgan was hypoglycemic. The practitioner instructed Morgan to stay away completely from sugars and other carbohydrates, and to eat a diet of strictly protein and vegetables, with small meals every few hours to stabilize her blood sugar.
At first, Morgan felt an improvement. She and Kim took this as an indication that the diet was helpful, so all through her early adult life, Morgan stayed clear of most carbs and all processed sugars. She focused on eating doctor-recommended proteins such as eggs, chicken, turkey, cheese, fish and nuts every few hours, as well as salads with tomatoes and cucumbers, which were allowed because they were low-carb. This gave Morgan the blood sugar and energy stability to function.
As she got into her late 20s, though, her energy levels became inconsistent again. She started to develop digestive gas and bloating, along with weight gain and fatigue. After exercising, she'd get a huge energy crash and intensely crave sugar.
Morgan had her blood drawn at the alternative doctor's office, and the A1C test showed evidence that she now had type-2 diabetes. She could barely process the information. She's hardly eaten any sugar over the last seven years. She read every food package, every label, and she studiously sought out protein and avoided carbohydrates. This had once seemed to be saving her.
Kim vented about the predicament to her hairdresser, who was a client of mine. She told Kim I'd be able to get to the bottom of Morgan's health problem.
Within the first minute of my phone call with Morgan and Kim, Spirit confirmed that Morgan was hypoglycemic and now technically had type-2 diabetes.
"How could this happen?" Morgan asked. "I strictly avoid sugar and carbs, and I eat protein every three hours."
"Sugar isn't the issue," I said. "It's fat. Unfortunately, Morgan, you were prescribed a high-fat diet under the guise of a high-protein one."
"I was told this was all protein I've been eating," Morgan said. "Where was the fat?"
"It was in the animal protein," I told her. "For seven years, fat has been your main calorie source, since you weren't living off sugar or carbohydrate calories."
"And why don't doctors know about this?"
"They haven't learned yet," I said. "They're wrapped up in the high-protein trend."
Kim cut in. "Why are these foods just called high-protein? Why isn't fat mentioned?"
"Because that's how it was first marketed back in the 1930s. If all these animal products were marketed as high-fat, they wouldn't have been as appealing."
I explained that the animal fat had burdened Morgan's liver and pancreas. "You felt stabilized for the first few years because you weren't going so long between meals, and because the high protein/high-fat combo had forced your adrenal glands to work harder, pumping out their energy hormones." Now, as she was getting older, she was exhibiting all the symptoms of adrenal fatigue and digestive distress, because her liver and pancreas had become sluggish. This was behind the weight gain, too.
"Your liver can't store glucose anymore to provide you with energy, and your adrenals are running low on adrenaline. We need to change your dietㅡlower your animal proteins to one serving at dinnertime, eliminate all dairy and eggs, and start bringing in natural sugars from fruit. And you need to let go of the carbohydrate fear that's been drilled into you. Bananas, apples, dates, grapes, melons, mangoes, pears, and berries are going to make every difference in your health. You can keep some nuts and seeds in rotation, just don't eat more than a handful once or twice daily."
Kim hesitated. "You're telling a diabetic that what she needs in her life is more sugar ?"
I hear this all the time. "Only the natural sugar in fruit," I said. I assured them both that if Morgan used the grazing technique and ate every two hours, using food combining to balance potassium, sodium, and sugar , as I described in Chapter 8, "Adrenal Fatigue:, she would do great. Any and all fruits and vegetables were wonderful components of those snack and meals. Suggested healing food combos for Morgan were celery or cucumbers with dates, apples, walnuts, or seeds.
Within the first month, Morgan felt more energy and emotional stability than she had in the last ten years. Her weight was going down, and she could finally exercise without collapsing afterward. Smoothies with dates, bananas, and celery became her favorite post-workout meal. And even though it seemed counter-intuitive to all advice on the diabetes front, she decided she was feeling so great with the change in diet that she only wanted one serving of animal protein a week.
Within four months, Morgan had reversed her type-2 diabetes. Her doctor was baffled as he presented the results of her A1C testㅡthat it was back to normal. In the months that followed, Morgan continued to restore her pancreas, liver, and adrenal glandsㅡand get her life back on track.
Over time, this damages the pancreas's ability to produce enough insulin to remove all the glucose it should from your bloodstream. And this under-performance alone is enough to create type-2 diabetes.
That's not the end of it. Your entire body is damaged by chronic floods of negative-emotion-based adrenaline. Especially if you eat when you're emotional, your pancreas will produce insulin that mixes with the adrenaline in your bloodstream, leading your body to associate the insulin with the fear-based adrenaline that's hurting it. Over time, this can make many of your cells "allergic" to your adrenaline/insulin blend and cause them to shun both hormones. Medical research has not yet uncovered this "Franken-sulin" hybrid ( as I call it), nor has it understood that the physical body revolts in this way. It's one of the primary causes of pancreatic weakness, which leads to lowered insulin production and nonacceptance of glucose in the body's cells.
Heavy, rich meals can trigger excess adrenaline production, too.That's because the adrenals are like a fire station, and fat triggers the alarm bell. When the adrenals get the signal that high levels of fat are in the bloodstreamㅡand therefore have the potential to put the pancreas and liver in immediate dangerㅡthe firehouse (the adrenals) sends out the fire trucks (adrenaline) to address the situation. That rush of adrenaline increase digestive strength to help move the fat through your system and protect you, but you pay a price, as this process can weaken the pancreas over time.
On the flip side, your adrenal glands may be under-performingㅡthat is, producing too little adrenaline. This makes your pancreas work overtime to try to compensate. If this condition is chronic, your pancreas will become inflamed or enlarged, and may eventually start under-performing as well.
Then again, you can have adrenal fatigue, in which your unstable adrenals are sometimes producing too little adrenaline and sometimes producing way too much. This can batter your pancreas as it becomes inflamed to compensate for dry spells of adrenaline and then gets scorched by floods of it.
Once your pancreas becomes dysfunctional, it can suffer damage from itself. That's because in addition to insulin, your pancreas produces enzymes that aid with digestion. Your pancreas also makes inhibitors that prevent these powerful enzymes from turning on itself as if it were a food to be dissolved. But if your pancreas grows sufficiently defective, it'll start under-producing its inhibitors, at which point the enzymes it produces will create even more damage. On top of that, you'll start experiencing digestive problems .....
A precursor to type-2 diabetes is a fluctuating but low glucose levelㅡcalled hypoglycemiaㅡwhich indicates a major issue with your body's ability to manage glucose properly. This can occur if your liver becomes impaired in its ability to store and release glucose. It can also happen if you're failing to eat at least a light, balanced snackㅡe.g., a fruit (for sugar and potassium) and a vegetable (for sodium)ㅡevery two hours. Regularly skipping meals forces your body to use up the liver's precious glucose storage, driving the body to run on adrenaline; and as previously mentioned, this can damage your pancreas, create insulin resistance, and lead to adrenal fatigue and weight gain over time.
One other major factor is the type of food you eat. There's a common misconception that diabetes is caused by eating a lot of foods with sugar in them. However, it's not actually the sugar that's the problem. It's sugar and fat combinedㅡmainly fat. For example, you could eat fruit all day and every day for the rest of your life and never get diabetes. In fact, eating a lot of fruit is the most effective way to add years to your life, as explained in Chapter 20, "Fruit Fear."
The problem is fat. Most people who consume processed foods and junk foods such as cakes, cookies, doughnuts, ice cream, and so onㅡor people who have a seemingly healthy main dish like chicken but follow it up with dessertㅡtypically eat a lot of fat and a lot of sugar at the same time. While sugar that's not attached to nutrients (e.g.,that isn't coming from fruit or vegetables) is definitely unhealthy, it's the fat that strains your liver and pancreas.
The first thing that will happen is that instant insulin resistance from the high levels of blood fat that result from an animal protein mealㅡwhether lean versions of pork, steak, or chicken, or fast food battered and fried in oilㅡwill stop the body's ability to allow the insulin produced by your pancreas to drive sugar into your cells. This will mean there's a whole lot of sugar floating around the bloodstream that can't go anywhere. A strong liver will help gather up as much glucose as it can to store for a rainy day. Over time, a diet high in animal fat, protein, and processed oils can burden the liver, though. Your liver can reach a vulnerable state from the constant responsibility to clean up the excess glucose in the bloodstream, and from waiting too many hours between meals to be refueled. When the liver becomes overburdened in this way, it dumps all of its glucose storage back into the bloodstream. This can prompt the birthing stage of hypoglycemia.
Since your liver has to take the burden of processing the fat you eat, a diet high in animal fat, which hides in even the lean animal protein people tend to think of as healthy, can make the organ sluggish and unable to store and release glucose the way it should. Large, heavy meals plus glucose dry spells caused by not eating in between can eventually result in type-2 diabetes.
At the same time, your pancreas has to produce enzymes to break down the fat so you can digest it. A lot of fat makes your pancreas work extra hard; and if you've already got other factors straining your pancreas, such as severe negative emotions and/or adrenal glands flooding it with corrosive adrenaline, a diet high in fat may be all that's needed to push your pancreas over the edge and create type-2 diabetes.
The good news is that all the damage described above is absolutely reversible. Next we'll cover how to heal your pancreas, your liver, and your insulin-traumatized cells so you can bring your hypoglycemia or type-2 diabetes to an end.
ADDRESSING TYPE-2 DIABETES AND HYPOGLYCEMIA
Since medical communities don't know the real story of what causes type-2 diabetes and hypoglycemia, they don't provide the proper diet guidance. Typically, they recommend a diet with little to no sugar in it, advising patients to avoid fruit altogether and focus on eating animal protein and vegetables.
Heeding this advice will probably keep you diabetic foreverㅡand not just diabetic and functional, but diabetic and ailingㅡ since the fat in meat is only going to make your condition worse, while eating fruit is critical for healing diabetes. It's imperative to understand that animal fats are what weakened the pancreas and liver to begin with.
Sugar was just the messenger. And in this case, health professionals shoot the messenger. That sugar was showcasing the insulin resistance that had cropped up from a pancreas overburdened by fat.
It's easy to eat a diet high in animal fat without realizingit. Even a lean-cut four-ounce piece of meat will contain a tablespoon of concentrated fat that can burden the pancreas and liver. So when a person is insulin resistant (even from a diet that seems traditionally "healthy") and puts sugar into her or his system, that sugar is going to prompt insulin problemsㅡand suddenly sugar is going to get all the attention, when it's NOT the real instigator.
Think of it like the teenager who throws a party when her parents are out of town. Say her younger brother drinks some punch-drink he didn't realize was spiked, gets sick, and calls Mum and Dad. Then say when they return home to a trashed house and drunk visitors, the big sister (fat) tries to blame the whole thing on her little brother (sugar). But he (sugar) didn't do anything wrong!
Now of course white table sugar and many other sweeteners aren't good for youㅡI'm not recommending you, eat these. Yet to address type-2 diabetes and hypoglycemia, it is critical to lower fat consumption and increase fresh fruit and vegetable consumption. I recommend the cleanse in Chapter 21 : The 28-Day Healing Cleanse to help heal the liver, pancreas, and adrenal glands and stabilize blood sugar levels.
Your doctor may prescribe insulin. While insulin lowers your blood glucose level, it does nothing to address core problems such as damaged adrenal glands, a damaged pancreas, a dysfunctional liver, chronic negative emotions, and/or insulin resistance.
What follows is a more targeted daily approach that focuses on healing every likely cause of your type-2 diabetes or hypoglycemia. You'll also find guidance in Part IV,"How to Finally Heal." How long you'll need to stick with this program depends on how much damage has to be undone. You should notice improvements within a few months, and the complete process typically requires six months to two-and-a-half years.
Bolster Your Adrenal Glands.
The fact that you have type-2 diabetes means it's likely you have an issue with your adrenal glands. Therefore, one step toward healing is to read Chapter 8, "Adrenal Fatigue." You can follow its advice to make your adrenal glands stable and strong.
Healing Foods
Wild blueberries, spinach, celery, papayas,sprouts, kale, raspberries, and asparagus are top foods to eat if you have type-2 diabetes or hypoglycemia. These perform functions such as detoxing the liver, strengthening glucose levels, supporting the pancreas, boosting the adrenal glands and stabilizing insulin.
Take care to avoid certain foods as well, most specifically cheese, milk, cream,butter, eggs, processed oils, and all sugars except raw honey and fruit.
Healing Herbs and Supplements
• Zinc: supports the pancreas and adrenal glands and helps stabilize glucose levels in the blood.
• Chromium: sustains the pancreas and adrenal glands and helps stabilze insulin levels.
• Spirulina (preferably from Hawaii): helps stabilize glucose levels in the blood and aids theadrenal glands.
• Ester-C: this form of vitamin C soothes and bolsters the adrenal glands.
• ALA (alpha lipoic acid): boosts the liver's ability to store and release glucose.
• Silica: helps stabilize the pancreas's release of insulin.
• Purslane: strengthens the pancreas and its production of digestive enzymes.
Health Benefits of Purslane. This wonderful green leafy vegetable is very low in calories (just 16 kcal/100g) and fats; nonetheless, it is rich in dietary fiber, vitamins, and minerals. Fresh leaves contain surprisingly more omega-3 fatty acids (α-linolenic acid) than any other leafy vegetable plant.
Purslane (Portulaca oleracea) or also known as cat's tongue provides many health benefits. It is good for our skin, urinary and digestive systems. It also has a perfect combination between antioxidants, omega 3 fatty acids, potassium, calcium, magnesium and carotene.
• Eleuthero (aka Siberian ginseng): enhances the body's ability to react and adapt, which helps prevent the adrenal glands from overreacting to fear, stress, and other intense emotions.
• Panax ginseng: also enhances the body's ability to react and adapt, which in turn helps prevent the adrenal glands from overreacting to fear, stress, and other intense emotions.
• EPA & DHA (eicosapentaenoic acid and docosahexaenoic acid): helps heal insulin resistance. be sure to buy a plant-based (not fish-based) version.
• Biotin: helps stabilize glucose levels in the blood and supports the central nervous system.
• B-complex: sustains the central nervous system.
• Gymnema sylvestre: helps lower glucose levels in the blood and stabilize insulin levels.
↑Gymnema is a woody climbing shrub native to India and Africa. The leaves are used to make medicine. Gymnema has a long history of use in India's Ayurvedic medicine. The Hindi name, gurmar, means "destroyer of sugar." Today, gymnema is used for diabetes, metabolic syndrome, weight loss, and cough.
• Magnesium: soothes digestive issues caused by an underperforming pancreas. Also calms stressed adrenal glands.
• Vitamin D3 : bolsters the pancreas and adrenal glands, and reduces inflammation. Vitamin D3 (cholecalciferol) is an essential vitamin that can be taken as a supplement to improve overall health or used for treating osteoporosis.
Vitamin D is sometimes called the “sunshine vitamin” because it’s produced in your skin in response to sunlight. It’s a fat-soluble vitamin in a family of compounds that includes vitamins D-1, D-2, and D-3.
Your body produces vitamin D naturally when it’s directly exposed to sunlight. You can also get it through certain foods and supplements to ensure adequate levels of the vitamin in your blood.
Vitamin D has several important functions. Perhaps the most vital are regulating the absorption of calcium and phosphorus, and facilitating normal immune system function. Getting a sufficient amount of vitamin D is important for normal growth and development of bones and teeth, as well as improved resistance against certain diseases.
If your body doesn’t get enough vitamin D, you’re at risk of developing bone abnormalities such as soft bones (osteomalacia) or fragile bones (osteoporosis).
Here are three more surprising benefits of vitamin D.
FIGHTS DISEASE
1. Vitamin D fights disease
In addition to its primary benefits, research suggests that vitamin D may also play a role in:
•reducing your risk of multiple sclerosis, according to a 2006 study published in the Journal of the American Medical Association
•decreasing your chance of developing heart disease, according to 2008 findings published in Circulation
•helping to reduce your likelihood of developing the flu, according to 2010 research published in the American Journal of Clinical Nutrition
REDUCES DEPRESSION
2. Vitamin D reduces depression
Research has shown that vitamin D might play an important role in regulating mood and warding off depression. In one study, scientists found that people with depression who received vitamin D supplements noticed an improvement in their symptoms.
In another study of people with fibromyalgia, researchers found vitamin D deficiency was more common in those who were also experiencing anxiety and depression.
BOOSTS WEIGHT LOSS
3. Vitamin D boosts weight loss
Consider adding vitamin D supplements to your diet if you’re trying to lose weight or prevent heart disease.
In one study, people taking a daily calcium and vitamin D supplement were able to lose more weight than subjects taking a placebo supplement. The scientists said the extra calcium and vitamin D had an appetite-suppressing effect.
In another study, overweight people who took a daily vitamin D supplement improved their heart disease risk markers.
VITAMIN D DEFICIENCY
Beware of D-ficiency
Many factors can affect your ability to get sufficient amounts of vitamin D through the sun alone. These factors include:
•Being in an area with high pollution
•Using sunscreen
•Spending more time indoors
•Living in big cities where buildings block sunlight
•Having darker skin. (The higher the levels of melanin, the less vitamin D the skin can absorb.)
These factors contribute to vitamin D deficiency in an increasing number of people. That’s why it’s important to get some of your vitamin D from sources besides sunlight.
The symptoms of a vitamin D deficiency in adults include:
•tiredness, aches and pains, and a general sense of not feeling well
•severe bone or muscle pain or weakness that may cause difficulty climbing stairs or getting up from the floor or a low chair, or cause you to walk with a waddling gait
•stress fractures, especially in your legs, pelvis, and hips
Doctors can diagnose a vitamin D deficiency by performing a simple blood test. If you have a deficiency, your doctor may order X-rays to check the strength of your bones.
If you’re diagnosed with a vitamin D deficiency, your doctor will likely recommend you take daily vitamin D supplements. If you have a severe deficiency, they may instead recommend high-dose vitamin D tablets or liquids. You should also make sure to get vitamin D through sunlight and the foods you eat.
Food sources of vitamin D
Few foods contain vitamin D naturally. Because of this, some foods are fortified. This means that vitamin D has been added. Foods that contain vitamin D include:
•salmon
•sardines
•egg yolk
•shrimp
•milk (fortified)
•cereal (fortified)
•yogurt (fortified)
•orange juice (fortified)
CASE HISTORY:
Getting a New Perspective on Sugar
Starting in her teens, Morgan battled what she called emotional highs and lows. Her mother, Kim, learned that if Morgan went too long without eating, she'd start to act out with a burst of frustration or fall into tears out of nowhere.
Kim repeatedly took Morgan to the family doctor to have her blood sugar levels evaluated, but Morgan's A1C and other tests would always come back normal. The doctor passed off Morgan's inconsistent behaviour as an aspect of being a sensitiveㅡor maybe even bipolarㅡgirl.
When Morgan was in her early 20s, Kim found an alternative doctor who said Morgan was hypoglycemic. The practitioner instructed Morgan to stay away completely from sugars and other carbohydrates, and to eat a diet of strictly protein and vegetables, with small meals every few hours to stabilize her blood sugar.
At first, Morgan felt an improvement. She and Kim took this as an indication that the diet was helpful, so all through her early adult life, Morgan stayed clear of most carbs and all processed sugars. She focused on eating doctor-recommended proteins such as eggs, chicken, turkey, cheese, fish and nuts every few hours, as well as salads with tomatoes and cucumbers, which were allowed because they were low-carb. This gave Morgan the blood sugar and energy stability to function.
As she got into her late 20s, though, her energy levels became inconsistent again. She started to develop digestive gas and bloating, along with weight gain and fatigue. After exercising, she'd get a huge energy crash and intensely crave sugar.
Morgan had her blood drawn at the alternative doctor's office, and the A1C test showed evidence that she now had type-2 diabetes. She could barely process the information. She's hardly eaten any sugar over the last seven years. She read every food package, every label, and she studiously sought out protein and avoided carbohydrates. This had once seemed to be saving her.
Kim vented about the predicament to her hairdresser, who was a client of mine. She told Kim I'd be able to get to the bottom of Morgan's health problem.
Within the first minute of my phone call with Morgan and Kim, Spirit confirmed that Morgan was hypoglycemic and now technically had type-2 diabetes.
"How could this happen?" Morgan asked. "I strictly avoid sugar and carbs, and I eat protein every three hours."
"Sugar isn't the issue," I said. "It's fat. Unfortunately, Morgan, you were prescribed a high-fat diet under the guise of a high-protein one."
"I was told this was all protein I've been eating," Morgan said. "Where was the fat?"
"It was in the animal protein," I told her. "For seven years, fat has been your main calorie source, since you weren't living off sugar or carbohydrate calories."
"And why don't doctors know about this?"
"They haven't learned yet," I said. "They're wrapped up in the high-protein trend."
Kim cut in. "Why are these foods just called high-protein? Why isn't fat mentioned?"
"Because that's how it was first marketed back in the 1930s. If all these animal products were marketed as high-fat, they wouldn't have been as appealing."
I explained that the animal fat had burdened Morgan's liver and pancreas. "You felt stabilized for the first few years because you weren't going so long between meals, and because the high protein/high-fat combo had forced your adrenal glands to work harder, pumping out their energy hormones." Now, as she was getting older, she was exhibiting all the symptoms of adrenal fatigue and digestive distress, because her liver and pancreas had become sluggish. This was behind the weight gain, too.
"Your liver can't store glucose anymore to provide you with energy, and your adrenals are running low on adrenaline. We need to change your dietㅡlower your animal proteins to one serving at dinnertime, eliminate all dairy and eggs, and start bringing in natural sugars from fruit. And you need to let go of the carbohydrate fear that's been drilled into you. Bananas, apples, dates, grapes, melons, mangoes, pears, and berries are going to make every difference in your health. You can keep some nuts and seeds in rotation, just don't eat more than a handful once or twice daily."
Kim hesitated. "You're telling a diabetic that what she needs in her life is more sugar ?"
I hear this all the time. "Only the natural sugar in fruit," I said. I assured them both that if Morgan used the grazing technique and ate every two hours, using food combining to balance potassium, sodium, and sugar , as I described in Chapter 8, "Adrenal Fatigue:, she would do great. Any and all fruits and vegetables were wonderful components of those snack and meals. Suggested healing food combos for Morgan were celery or cucumbers with dates, apples, walnuts, or seeds.
Within the first month, Morgan felt more energy and emotional stability than she had in the last ten years. Her weight was going down, and she could finally exercise without collapsing afterward. Smoothies with dates, bananas, and celery became her favorite post-workout meal. And even though it seemed counter-intuitive to all advice on the diabetes front, she decided she was feeling so great with the change in diet that she only wanted one serving of animal protein a week.
Within four months, Morgan had reversed her type-2 diabetes. Her doctor was baffled as he presented the results of her A1C testㅡthat it was back to normal. In the months that followed, Morgan continued to restore her pancreas, liver, and adrenal glandsㅡand get her life back on track.

No comments:
Post a Comment