 Before starting these techniques, ask your Health Care Provider if they are right for you.
Before starting these techniques, ask your Health Care Provider if they are right for you.
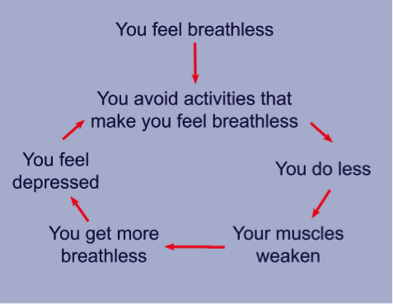
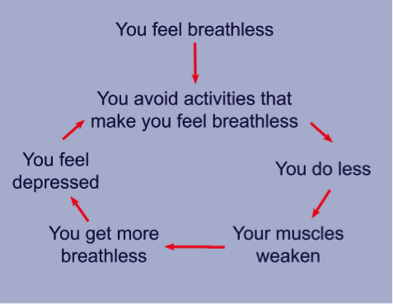
Having COPD makes it harder to breathe. And when it’s hard to breathe, it’s normal to get anxious, making you feel even more short of breath. Chronic Obstructive Pulmonary Disease (COPD) is an umbrella term used to describe progressive lung diseases including emphysema, chronic bronchitis, refractory (non-reversible) asthma, and some forms of bronchiectasis.
There are two breathing techniques that can help you get the air you need without working so hard to breathe: Pursed-lips Breathing and Diaphragmatic (also called Belly or Abdominal) Breathing.
Better Breathing Tip: It’s normal to hold your shoulders tense and high. Before starting any breathing technique, take a minute to drop your shoulders down, close your eyes, and relax.
Pursed-Lips Breathing
- Slows your breathing down
- Keeps airways open longer so your lungs can get rid of more stale, trapped air
- Reduces the work of breathing
- Increases the amount of time you can exercise or perform an activity
- Improves the exchange of oxygen and carbon dioxide
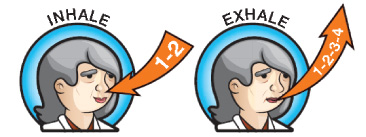
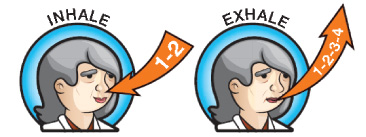
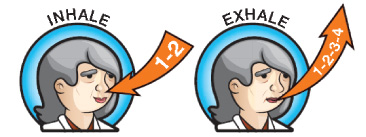
To do purse-lips breathing:
- Breathe in through your nose (as if you are smelling something) for about 2 seconds.
- Pucker your lips like you’re getting ready to blow out candles on a birthday cake.
- Breathe out very slowly through pursed-lips, two to three times as long as you breathed in.
- Repeat.
Diaphragmatic (Abdominal/Belly) Breathing
The diaphragm is the main muscle of breathing. It’s supposed to do most of the work. When you have COPD, the diaphragm doesn’t work as well and muscles in the neck, shoulders and back are used. These muscles don’t do much to move your air. Training your diaphragm to take over more “work of breathing” can help.
Diaphragmatic breathing is not as easy to do as pursed-lips breathing. It is recommended that you get instruction from a respiratory health care professional or physical therapist experienced in teaching it.
This technique is best used when you’re feeling rested and relaxed, and while sitting back or lying down.
- Relax your shoulders.
- Place one hand on your chest and the other on your belly.
- Inhale through your nose for about two seconds.
- As you breathe in, your belly should move outward. Your belly should move more than your chest.
- As you breathe out slowly through pursed-lips, gently press on your belly. This will push up on your diaphragm to help get your air out.
- Repeat.
Better Breathing Tip: Stop, Reset, Continue
When you are feeling short of breath during exercise or regular activities, use these 3 steps:
- Stop your activity.
- Reset by sitting down, relax your shoulders, and do pursed-lips breathing until you catch your breath.
- Continue activity, doing pursed-lips breathing as you go. Go at a slower pace if you need to.
Staying Healthy and Avoiding Pneumonia
What is pneumonia?
Pneumonia is an infection of one or both lungs. Organisms settle in the air sacs where they grow rapidly. These air sacs become filled with pus and fluid as the body attempts to fight infection. Young children, cigarette smokers, adults over 65 and people with certain medical problems including COPD are at greater risk for developing pneumonia. COPD is the third leading cause of death, while pneumonia and flu contribute to the eighth leading cause of death in the United States.
What causes pneumonia?
Pneumonia is most commonly caused by bacteria, viruses and less commonly fungi which are more common in patients with suppressed immune systems. Contact with the organisms occurs either through directly touching objects with your hands (which then transmit the organism to your mouth, nose or eyes), or through inhalation of droplets containing the organisms. The causes of pneumonia for which vaccines (shots) are available include:
- Influenza (Flu)
- Pneumococcus
- Measles
- Pertussis (whooping cough)
- Haemophilus influenzae type b (Hib)
Symptoms of pneumonia:
There are several symptoms of pneumonia that are similar to those of a COPD flare-up, which are often caused by infection. It is important to recognize these pneumonia symptoms and to call your doctor if you experience one or more of the following:
- Fever over 100.5 degrees or shaking chills
- Shortness of breath or more rapid breathing
- Nausea, vomiting or diarrhea
- Cough with increased amount of mucus
- Cough with a change in mucus color
- More rapid heart rate
- Pain in one area of the chest with deep breaths
How can I avoid pneumonia?
- See your health care professional at your regularly scheduled appointment even if you feel fine
- Get your flu shot every year. Local pharmacies and grocery stores offer these shots at the start of flu season
- Check if you are due for a pneumonia shot which can greatly reduce your risk of developing pneumonia
- Wash your hands often and carry a small bottle of hand sanitizer for when you cannot wash your hands
- Avoid touching your mouth, eyes, and nose in public to help prevent germs from entering your body
- Stay away from crowds, especially during cold and flu season
- Use your own pen, especially when signing in at your doctor’s office or other health care appointments
- Don’t smoke as it makes it harder for the lungs to fight off an infection
- Get plenty of sleep. When your body is tired, you're more likely to get sick
It is possible to stay healthy, even if you have COPD, at any stage. Watch for early warning signs of COPD flare-ups which may include pneumonia and report them right away. Work with your health care team to avoid pneumonia!
 Our Body of Water
The majority of the body is made up of water with up to 75% of the
body's weight due to H2O. Most of the water is found within the
cells of the body (intracellular space). The rest is found in the
extracellular space, which consists of the blood vessels
(intravascular space) and the spaces between cells (interstitial
space).
Our Body of Water
The majority of the body is made up of water with up to 75% of the
body's weight due to H2O. Most of the water is found within the
cells of the body (intracellular space). The rest is found in the
extracellular space, which consists of the blood vessels
(intravascular space) and the spaces between cells (interstitial
space).
 What is Dehydration?
Dehydration occurs when the amount of water leaving the body is
greater than the amount being taken in. The body is very dynamic
and always changing. This is especially true with water levels in
the body. We lose water routinely when we:
>breathe and humidified air leaves the body;
>sweat to cool the body; and
>urinate or have a bowel movement to rid the body of waste
products.
What is Dehydration?
Dehydration occurs when the amount of water leaving the body is
greater than the amount being taken in. The body is very dynamic
and always changing. This is especially true with water levels in
the body. We lose water routinely when we:
>breathe and humidified air leaves the body;
>sweat to cool the body; and
>urinate or have a bowel movement to rid the body of waste
products.
In a normal day, a person has to drink a significant amount of
water to replace this routine loss.

Causes of Dehydration: Diarrhea.
Diarrhea is the most common reason a person loses excess
water. Diarrhea consists of unusually frequent or unusually liquid
bowel movements and excessive watery evacuations of fecal material. Persistent diarrhea is both uncomfortable and dangerous, as a significant amount of water can be lost with each
bowel movement. Worldwide, more than four million children die
each year because of dehydration from diarrhea.
 Causes of Dehydration: Vomiting
Vomiting is the act of forcible emptying of the stomach, in which
the stomach has to overcome the pressures that are normally in
place to keep food and secretions within the stomach. The
stomach almost turns itself inside out - forcing itself into the
lower portion of the esophagus (the tube that connects the mouth
to the stomach) during a vomiting episode. Constant vomiting can
be a serious cause of fluid loss and it is difficult for a person to
replace water if they are unable to tolerate liquids.
Causes of Dehydration: Vomiting
Vomiting is the act of forcible emptying of the stomach, in which
the stomach has to overcome the pressures that are normally in
place to keep food and secretions within the stomach. The
stomach almost turns itself inside out - forcing itself into the
lower portion of the esophagus (the tube that connects the mouth
to the stomach) during a vomiting episode. Constant vomiting can
be a serious cause of fluid loss and it is difficult for a person to
replace water if they are unable to tolerate liquids.
 Causes of Dehydration: Sweat
The body can lose significant amounts of water when it tries to
cool itself by sweating. Whether the body is hot because of the
environment (for example, working in a warm environment),
intense exercising in a hot environment, or because a fever is
present due to an infection; the body uses a significant amount of
water in the form of sweat to cool itself. Depending upon weather
conditions, a brisk walk will generate up to 16 ounces of sweat
(one pound of water).
Causes of Dehydration: Sweat
The body can lose significant amounts of water when it tries to
cool itself by sweating. Whether the body is hot because of the
environment (for example, working in a warm environment),
intense exercising in a hot environment, or because a fever is
present due to an infection; the body uses a significant amount of
water in the form of sweat to cool itself. Depending upon weather
conditions, a brisk walk will generate up to 16 ounces of sweat
(one pound of water).
 Causes of Dehydration: Diabetes
In people with diabetes, elevated blood sugar levels cause sugar
to spill into the urine, and water then follows, which can cause
significant dehydration. For this reason, frequent urination and
excessive thirst are among the symptoms of diabetes.
Causes of Dehydration: Diabetes
In people with diabetes, elevated blood sugar levels cause sugar
to spill into the urine, and water then follows, which can cause
significant dehydration. For this reason, frequent urination and
excessive thirst are among the symptoms of diabetes.
 Causes of Dehydration: Burns
The skin has an important role to play in the fluid and temperature
regulation of the body. If enough skin area is injured, the ability to maintain that control can be lost. Burn victims become
dehydrated because water seeps into the damaged skin. Other
inflammatory diseases of the skin are also associated with fluid
loss.
Causes of Dehydration: Burns
The skin has an important role to play in the fluid and temperature
regulation of the body. If enough skin area is injured, the ability to maintain that control can be lost. Burn victims become
dehydrated because water seeps into the damaged skin. Other
inflammatory diseases of the skin are also associated with fluid
loss.
 Causes of Dehydration: Inability to Drink Fluids
The inability to drink adequately is another potential cause of
dehydration. Whether it is the lack of availability of water or the
lack of strength to drink adequate amounts, this, coupled with
routine or excessive amounts of water loss can compound the
degree of dehydration.
Causes of Dehydration: Inability to Drink Fluids
The inability to drink adequately is another potential cause of
dehydration. Whether it is the lack of availability of water or the
lack of strength to drink adequate amounts, this, coupled with
routine or excessive amounts of water loss can compound the
degree of dehydration.
 What Are the Signs and Symptoms of Dehydration?
What Are the Signs and Symptoms of Dehydration?
The body's initial responses to dehydration are thirst to increase
water intake along with decreased urine output to try to conserve
water. The urine will become concentrated and more yellow in
color. As the level of water loss increases, more symptoms can
become apparent, such as increased thirst, dry mouth, cessation
of tear production by the eyes, cessation of sweating , muscle
cramps, nausea and vomiting, heart palpitations, and
lightheadedness (especially when standing). With severe
dehydration, confusion and weakness will occur as the brain and
other body organs receive less blood. Finally, coma and organ
failure will occur if the dehydration remains untreated.
 How is Dehydration Diagnosed?
Dehydration is often a clinical diagnosis. Aside from diagnosing
the reason for dehydration, the health care professional's
examination of the patient will assess the level of dehydration.
Initial evaluations may include:
Mental status tests to evaluate whether the patient is awake,
alert, and oriented.
Vital sign assessments may include postural readings
(blood pressure and pulse rate are taken lying down and
standing). With dehydration, the pulse rate may increase and
the blood pressure may drop because the intravascular
space is depleted of water.
Temperature may be measured to assess fever.
Skin will be checked to see if sweat is present and to assess
the degree of elasticity. As dehydration progresses, the skin
loses its water content and becomes less elastic.
Infant evaluation: infants may have additional evaluations
performed, including checking for a soft spot on the skull
(sunken fontanelle), assessing the suck mechanism, muscle,tone, or loss of sweat in the armpits and groin.
How is Dehydration Diagnosed?
Dehydration is often a clinical diagnosis. Aside from diagnosing
the reason for dehydration, the health care professional's
examination of the patient will assess the level of dehydration.
Initial evaluations may include:
Mental status tests to evaluate whether the patient is awake,
alert, and oriented.
Vital sign assessments may include postural readings
(blood pressure and pulse rate are taken lying down and
standing). With dehydration, the pulse rate may increase and
the blood pressure may drop because the intravascular
space is depleted of water.
Temperature may be measured to assess fever.
Skin will be checked to see if sweat is present and to assess
the degree of elasticity. As dehydration progresses, the skin
loses its water content and becomes less elastic.
Infant evaluation: infants may have additional evaluations
performed, including checking for a soft spot on the skull
(sunken fontanelle), assessing the suck mechanism, muscle,tone, or loss of sweat in the armpits and groin.
Pediatric patients are often weighed during routine visits, thus a body weight measurement may be helpful in assessing how much water has been lost with the acute illness.
In some cases, blood tests to measure potential electrolyte abnormalities and urinalysis may be ordered to determine the level of dehydration in the patient.
 How is Dehydration Treated?
How is Dehydration Treated?
Fluid replacement is the treatment for dehydration. This may be
attempted by replacing fluid by mouth, but if this fails, intravenous
fluid (IV) may be required. Should oral rehydration be attempted,
frequent small amounts of clear fluids should be used.
Clear fluids include:
>water,
>clear broths,
>popsicles,
>Jell-O, and
>other replacement fluids that may contain electrolytes.
Can Dehydration Be Treated at Home?
Dehydration occurs over time. If it can be recognized in its earliest
stages, and if its cause can be addressed, then home treatment may be adequate. Steps a person can take at home to prevent
severe dehydration include:
>People with vomiting and diarrhea can try to alter their diet
and use water-cure-protocol formula to control symptoms to minimize water loss.
>Acetaminophen or ibuprofen may be used to control fever.
Ibuprofen may irritate the stomach and cause nausea and
vomiting, so it should be used with caution in individuals
who already have these symptoms.
>Fluid replacements may be attempted by replacing fluid by mouth with frequent small amounts of clear fluids.
If the individual becomes confused or lethargic; if there is
persistent, uncontrolled fever, vomiting, or diarrhea; or if there are
any other specific concerns, then medical care should be accessed. EMS or 911 should be activated for any person with altered mental status.
 What Are the Complications of Dehydration?
What Are the Complications of Dehydration?
Complications of dehydration may occur because of the
dehydration, and/or because of the underlying disease or situation
that causes the fluid loss. Complications that may occur include:
>kidney failure,
>coma,
>shock,
>heat-related illnesses (heat exhaustion or heat stroke), and
>electrolyte abnormalities.
 Dehydration Prevention Tip #1
Dehydration Prevention Tip #1
Plan ahead and take extra water to all outdoor events where
increased sweating, activity, and heat stress will increase fluid
loss. Encourage athletes and people who work outside to replace
fluids at a rate that equals the loss.
 Dehydration Prevention Tip #2
Dehydration Prevention Tip #2
Check weather forecasts for high heat index days. When
temperatures are high, avoid exercise, outdoor exposure, and plan
events that must occur outside during times of the day when
temperatures are lower.
 Dehydration Prevention Tip #3
Dehydration Prevention Tip #3
The young and elderly are most at risk of dehydration. Ensure that
older people, infants, and children have adequate drinking water or
fluids available and assist them as necessary. Encourage
individuals who are incapacitated or impaired to drink plenty of
water and assure they are provided with adequate fluids.
During heat waves, attempts should be made to check on the elderly in their homes. During the Chicago heat wave of 1995, more than 600 people died in their homes from heat exposure.
 Dehydration Prevention Tip #4
Dehydration Prevention Tip #4
Avoid alcohol consumption, especially when it is very hot, because
alcohol increases water loss and impairs your ability to recognize
early signs associated with dehydration.
 Dehydration Prevention Tip #5
Dehydration Prevention Tip #5
Wear light-colored and loose-fitting clothing if you must be
outdoors when it is hot outside. Drink plenty of water and carry a
personal fan or mister to cool yourself.
 Dehydration Prevention Tip #6
Dehydration Prevention Tip #6
Break up your exposure to hot temperatures. Find air-conditioned
or shady areas and allow yourself to cool between exposures.
Taking someone into a cooled area for even a couple of hours
each day will help prevent the cumulative effects of high heat
exposure.
 Dehydration Prevention Tip #7
Dehydration Prevention Tip #7
Know the signs and symptoms of heat cramps, heat rash, heat
exhaustion, and heat stroke. Preventing dehydration is one step to
avoid these conditions.
 Dehydration At A Glance
Dehydration At A Glance
>The body needs water to function.
>Dehydration occurs when water intake is less than water loss.
>Symptoms range from mild to life-threatening.
>Prevention is the important first step in treating dehydration.
>The young and the elderly are especially susceptible to
dehydration.
How is dehydration diagnosed?
Dehydration is often a clinical diagnosis. Aside from diagnosing the reason for dehydration, the health care professional's examination of the patient will assess the level of dehydration. Initial evaluations may include:
Mental status tests to evaluate whether the patient is awake, alert, and oriented. Infants and children may appear listless and have whiny cries and decreased muscle tone.
Vital signs may include postural readings (blood pressure and pulse rate are taken lying down and standing). With dehydration, the pulse rate may increase and the blood pressure may drop because the blood is depleted of fluid. People taking beta blocker medications for high blood pressure, heart disease, or other indications, occasionally lose the ability to increase their heart rate as a compensation mechanism since these medications block the adrenaline receptors in the body.
Temperature may be measured to assess fever. While it is common to measure temperature in the ear (tympanic) or by mouth (orally), a rectal thermometer may be used to assess core body temperature if the patient appears warm, but no fever is noted tympanically or orally.
Skin may be checked to see if sweat is present and to assess the degree of elasticity (turgor). As dehydration progresses, the skin loses its water content and becomes less elastic. The amount of sweat is often felt in the armpit or groin, two areas that tend to have moisture normally.
The mouth can become dry and the health care professional may look at or feel the tongue to see how wet it is.
Infants may have additional evaluations performed, including checking for a soft spot on the skull (sunken fontanelle), and assessing the suck mechanism, loss of sweat in the armpits and groin, and muscle tone. All are signs of potential significant dehydration.
Pediatric patients are often weighed during routine child visits, thus a body weight measurement may be helpful in assessing how much water has been lost with the acute illness. This is very rough estimate because all scales are not the same, and for infants and children, it is important to know what clothing they were wearing when the original weight was taken.
Laboratory testing
The purpose of blood tests is to assess potential electrolyte abnormalities (including sodium, potassium, chloride, and carbon dioxide levels) associated with the dehydration. Other tests may or may not be ordered depending upon the underlying cause of dehydration, the severity of illness, and the health care professional's assessment of their needs and resources available.
Other blood tests may be helpful in determining the level of dehydration. Hemoglobin and red blood cell counts may be elevated because the blood is more concentrated with water loss from the intravascular space.
Kidney function tests including BUN and creatinine may be elevated, and this is one way of measuring the severity of dehydration.
Urinalysis may be ordered to determine urine concentration; the more concentrated the urine, the more dehydrated the patient.