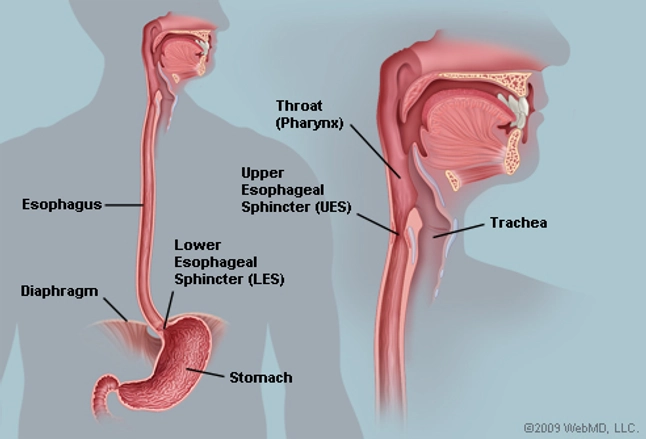
The esophagus is a muscular tube connecting the throat (pharynx) with the stomach. The esophagus is about 8 inches long, and is lined by moist pink tissue called mucosa. The esophagus runs behind the windpipe (trachea) and heart, and in front of the spine. Just before entering the stomach, the esophagus passes through the diaphragm.
The upper esophageal sphincter (UES) is a bundle of muscles at the top of the esophagus. The muscles of the UES are under conscious control, used when breathing, eating, belching, and vomiting. They keep food and secretions from going down the windpipe.
The lower esophageal sphincter (LES) is a bundle of muscles at the low end of the esophagus, where it meets the stomach. When the LES is closed, it prevents acid and stomach contents from traveling backwards from the stomach. The LES muscles are not under voluntary control.
Click here to watch video: This video is of an esophagoscopy in a 3-year-old child. The esophagoscope is introduced through the mouth. As the scope enters the esophageal inlet, the larynx becomes visible with an endotracheal tube passing through the vocal folds. The esophagoscope meets some resistance as it is passed through the upper esophageal sphincter. The esophagus is then entered, and the mucosal lining of the esophagus is evaluated. The esophagus is then passed through the lower esophageal sphincter, entering the stomach. The rugae of the stomach are very distinct. The pylorus is visualized first, and then the scope is turned 180º, and the lower esophageal sphincter is visualized. The scope is visible coming through the lower esophageal sphincter. Video courtesy of Ravindhra G Elluru, MD, PhD.
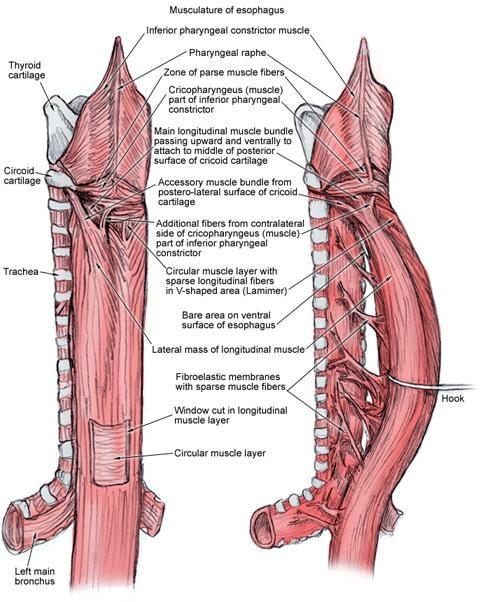
The esophagus has 3 constrictions in its vertical course, as follows:
- The first constriction is at 15 cm from the upper incisor teeth, where the esophagus commences at the cricopharyngeal sphincter; this is the narrowest portion of the esophagus and approximately corresponds to the sixth cervical vertebra
- The second constriction is at 23 cm from the upper incisor teeth, where it is crossed by the aortic arch and left main bronchus
These measurements are clinically important for endoscopy and endoscopic surgeries of the esophagus.
The esophagus has been subdivided into 3 portions, as follows:
- The cervical portion extends from the cricopharyngeus to the suprasternal notch
- The thoracic portion extends from the suprasternal notch to the diaphragm
Relationships of the esophagus
The relationships of the cervical esophagus, thoracic esophagus, and abdominal esophagus are described below. [1, 2]
Blood supply
See the list below:
- The cervical portion is supplied by the inferior thyroid artery
- The thoracic portion is supplied by bronchial and esophageal branches of the thoracic aorta
- The abdominal portion is supplied by ascending branches of the left phrenic and left gastric arteries.
Venous drainage
Venous blood from the esophagus drains into a submucosal plexus. From this plexus, blood drains to the periesophageal venous plexus. Esophageal veins arise from this plexus and drain in a segmental way similar to the arterial supply, as follows:- From the cervical esophagus, veins drain into the inferior thyroid vein
- From the thoracic esophagus, veins drain into the azygos veins, hemiazygos, intercostal, and bronchial veins
- From the abdominal portion, esophagus veins drain into the left gastric vein; the left gastric vein is a tributary of the portal system.
Lymphatic drainage
The esophagus has an extensive, longitudinally continuous, submucosal lymphatic system. The esophagus has 2 types of lymphatic vessels. A plexus of large vessels is present in the mucous membrane, and it is continuous above with the mucosal lymphatic vessels of pharynx and below with mucosal lymphatic vessels of gastric mucosa. The second plexus of finer vessels is situated in the muscular coat. Efferent vessels from the cervical part drain into the deep cervical nodes. Vessels from the thoracic part drain to the posterior mediastinal nodes and from the abdominal part drain to the left gastric nodes. Some vessels may pass directly to the thoracic duct.Lymphatic drainage of the esophagus contains little barrier to spread, and esophageal lymphatics are densely interconnected. Hence, esophagus carcinoma can spread through the length of the esophagus via lymphatics and may have nodal involvement several centimeters away from the primary lesion.
Nerve supply
Recurrent laryngeal branches of the vagus nerve supply the striated muscle in the upper third of the esophagus, and cell bodies for these fibers are situated in the rostral part of the nucleus ambiguus. Motor supply to the nonstriated muscle is parasympathetic, and cell bodies for these fibers are situated in the dorsal nucleus of vagus. These fibers reach the esophagus through the vagus and its recurrent laryngeal branches. They synapse in the esophagus wall in the ganglia of submucosal plexus (Meissner) and myenteric plexus (Auerbach). The myenteric is situated between the outer longitudinal and inner circular muscle fibers. From these plexuses, short, postganglionic fibers emerge to innervate the mucous glands and smooth muscle fibers within the walls of the esophagus.Vasomotor sympathetic fibers that supply the esophagus arise from the upper 4-6 thoracic spinal cord segments. Fibers from the upper ganglia pass to the middle and inferior cervical ganglia and synapse on postganglionic neurons. The axons of these neurons innervate the vessels of the cervical and upper thoracic esophagus. Postsynaptic fibers from the lower ganglia pass to the esophageal plexus to innervate the distal esophagus. Afferent visceral pain fibers travel via the sympathetic fibers to the first 4 segments of the thoracic spinal cord.
Esophagus Conditions
- Heartburn: An incompletely closed LES allows acidic stomach contents to back up (reflux) into the esophagus. Reflux can cause heartburn, cough or hoarseness, or no symptoms at all.
- Gastroesophageal reflux disease (GERD): When reflux occurs frequently or is bothersome, it's called gastroesophageal reflux disease (GERD).
- Esophagitis: Inflammation of the esophagus. Esophagitis can be due to irritation (as from reflux or radiation treatment) or infection.
- Barrett's esophagus: Regular reflux of stomach acid irritates the esophagus, which may cause the lower part to change its structure. Very infrequently, Barrett's esophagus progresses to esophageal cancer.
- Esophageal ulcer: An erosion in an area of the lining of the esophagus. This is often caused by chronic reflux.
- Esophageal stricture: A narrowing of the esophagus. Chronic irritation from reflux is the usual cause of esophageal strictures.
- Achalasia: A rare disease in which the lower esophageal sphincter does not relax properly. Difficulty swallowing and regurgitation of food are symptoms.
- Esophageal cancer: Although serious, cancer of the esophagus is uncommon. Risk factors for esophageal cancer include smoking, heavy drinking, and chronic reflux.
- Mallory-Weiss tear: Vomiting or retching creates a tear in the lining of the esophagus. The esophagus bleeds into the stomach, often followed by vomiting blood.
- Esophageal varices: In people with cirrhosis, veins in the esophagus may become engorged and bulge. Called varices, these veins are vulnerable to life-threatening bleeding.
- Esophageal ring (Schatzki's ring): A common, benign accumulation of tissue in a ring around the low end of the esophagus. Schatzki's rings usually cause no symptoms, but may cause difficulty swallowing.
- Esophageal web: An accumulation of tissue (similar to an esophageal ring) that usually occurs in the upper esophagus. Like rings, esophageal webs usually cause no symptoms.
- Plummer-Vinson syndrome: A condition including chronic iron-deficient anemia, esophageal webs, and difficulty swallowing. Iron replacement and dilation of esophageal webs are treatments.
- Esophageal stricture: A narrowing of the esophagus, from a variety of causes, which, if narrow enough, may lead to difficult swallowing.
Esophagus Tests
- Upper endoscopy, EGD (esophagogastroduodenoscopy): A flexible tube with a camera on its end (endoscope) is inserted through the mouth. The endoscope allows examination of the esophagus, stomach, and duodenum (small intestine).
- Esophageal pH monitoring: A probe that monitors acidity (pH) is introduced into the esophagus. Monitoring pH can help identify GERD and follow the response to treatment.
- Barium swallow: A person swallows a barium solution, then X-ray films are taken of the esophagus and stomach. Most often, a barium swallow is used to seek the cause of difficulty swallowing
Esophagus Treatments
- H2 blockers: Histamine stimulates acid release in the stomach. Certain antihistamines called H2 blockers can reduce acid, improving GERD and esophagitis.
- Proton pump inhibitors: These medicines turn off many of the acid-producing pumps in the stomach wall. Reduced stomach acid can reduce GERD symptoms, and help ulcers or esophagitis to heal.
- Esophagectomy: Surgical removal of the esophagus, usually for esophageal cancer.
https://www.bostonscientific.com/content/dam/bostonscientific/endo/general/gastro-specialty/eso_stent_patient_nutrition.pdf

An esophageal stent is a flexible mesh tube, approximately
2cm (3/4 inch) wide, and is placed through the constricted
area of your esophagus (food tube) to allow food and
beverages to pass from your mouth to your stomach for
digestion and absorption of nutrients.
The stent gently expands to hold the narrowed area of
the esophagus open and should make swallowing foods
and beverages easier. The stent will not be as wide or as
flexible as a normal esophagus so you will need to take
care with certain foods and in the way you eat to prevent
blocking the stent.
This is an example of what your stent may look like:
‹ Esophagus
‹ Esophageal Stricture or Tumor
‹ Esophageal Stent
‹ Stomach
Fluids only – water, tea, coffee, fruit juices, milk,
soft drinks or sports drinks.
Start with small sips and increase the volume as
you feel confident.
Smooth or pureed foods, including soup (without
lumps), applesauce, yogurt, ice cream, pudding
or gelatin.
Increase the texture of your food to a soft
consistency as you feel your swallowing becomes
easier and your confidence builds. You may try
scrambled eggs, cottage cheese, steamed fish,
mashed potatoes, mashed banana and pudding.
Try to include a wide variety of foods and fluids
in your diet so you achieve as close to a normal
diet as possible and to ensure you meet your
nutritional needs. If you feel that you cannot
achieve this on a soft consistency diet, ask to
speak to a registered dietitian.
For meal suggestions, please refer to the last two
pages of this brochure.
What can I eat?
Once the stent has been placed, your medical team will
advise you on when it is safe to start eating and drinking
again. You will start with fluids and then build up gradually
to a soft diet. It can take one to two days for the stent to
fully expand so take it slowly initially.
Your healthcare team will let you know how quickly to
progress through the following dietary stages:
Stage 2
Are there any foods
I should avoid?
The stent has been placed to allow you to eat as normally
as possible. However, it is possible for the stent to become
blocked. The most common reason for stents to block is
from food that is swallowed without being sufficiently
chewed or from foods that do not break down enough
when chewed.
The following foods can be difficult to break down, despite
chewing, and so are more likely to cause your stent to
become blocked:
Bread and toast
Tough gristly meat
Hard boiled or fried egg
Fish with bones
Pithy fruit (e.g., orange, grapefruit, pineapple)
Stringy vegetables (e.g., green beans, celery)
Potato skins
Salad items (e.g., salad leaves and lettuce)
Raw vegetables
Chips
Ice cream or yogurt with chunks of fruit, cereal or nuts
To minimize the risk of blocking the stent, it is important
to think about the foods that you are eating. Some foods,
when chewed well, will be easier to swallow than others.
For example, bread sticks will crumble when chewed but
bread will form a sticky lump.
How can I prevent
blocking the stent?
Take your time, relax and eat your meals slowly.
Meals should be smaller than you are used to and
more frequent – aim for five or six small meals rather
than three big meals.
Cut your food into smaller pieces than you would
normally eat, take small mouthfuls and chew each
mouthful thoroughly.
Don’t be afraid to spit out lumps that can’t be chewed.
Have plenty of sauces, gravy or cream with your meals.
It will make your food moist, therefore easier to
swallow and pass through your stent.
Take frequent drinks during and after each meal to help
keep your stent clear. Warm or carbonated beverages
are recommended, but all fluids are beneficial. For some
people, carbonation may worsen symptoms of heartburn
or acid reflux.
Sit upright at meal times and for one to two hours
afterwards.
If you wear dentures, make sure they fit correctly, so you
can chew your food well.
Ask your healthcare team about pills that are hard
to swallow.
Ask if any of your pills are available in liquid form.
Ask your pharmacist if crushing your pills is an
option, as some pills may become less effective
when crushed.
Pills that can be crushed can be added to applesauce
or other soft foods.
Remember it is important to include a
wide variety of foods of suitable texture to
give you all the nourishment you need.
Esophageal Stent Placement
This information explains your esophageal stent placement, including how to prepare for your procedure and how to care for yourself after your procedure.
About Esophageal Stents
Your esophagus (food pipe) is the tube that carries food and liquids, including saliva, from your mouth to your stomach when you swallow. Esophageal cancer (cancer of your esophagus) can make it hard to swallow. This is called dysphagia.In order to make it easier for you to swallow, your doctor has recommended that you get an esophageal stent. This is a hollow tube that’s placed in your esophagus in the area of the tumor to hold the area open.
Esophageal stents are inserted through your mouth, and no surgery is needed. Most people return home on the same day as their procedure. However, some people are admitted to the hospital after their procedure for observation.
Having a stent won’t affect your ability to receive cancer treatment such as chemotherapy or radiation therapy.
1 Week Before Your Procedure
Ask about your medications
You may need to stop taking or change the dose of some of your medications before your procedure. Talk with your doctor if you take any of the medications below.Anticoagulants (blood thinners)
If you take medication to thin your blood, such as to treat blood clots or to prevent a heart attack or stroke, ask the doctor who prescribes it when to stop taking it. See below for examples of blood thinners.
|
|
Medications for diabetes
If you take insulin or other medications for diabetes, you may need to change the dose. Ask the doctor who prescribes your diabetes medication what you should do the day before and the morning of your procedure.If you take metformin (such as Glumetza®) or a medication that contains metformin, don’t take it the day before or the day of your procedure.
Get a letter from your doctor, if needed
- If you have an automatic implantable cardioverter-defibrillator (AICD), you need to get a clearance letter from your cardiologist (heart doctor) before your procedure.
- If you’ve had chest pain, trouble breathing that’s new or worse, or have fainted in the last 6 weeks, you will need to get a clearance letter from your doctor before your procedure.
- Your MSK doctor’s office must receive your clearance letter(s) at least 1 day before your procedure.
Arrange for someone to take you home
You must have someone 18 years or older take you home after your procedure.3 Days Before Your Procedure
An endoscopy nurse will call you between 8 am and 6 pm 3 days before your procedure. The nurse will review the instructions in this guide with you and ask you questions about your medical history. The nurse will also review your medications and tell you which medications to take the morning of your procedure. Use the space below to write them down.The Day Before Your Procedure
Instructions for eating and drinking before your surgery
- Do not eat anything after midnight the night before your surgery. This includes hard candy and gum.
- Between midnight and up until 2 hours before your scheduled arrival time, you may drink a total of 12 ounces of water (see figure).
- Starting 2 hours before your scheduled arrival time, do not eat or drink anything. This includes water.
The Day of Your Procedure
Things to remember
- Take only the medications you were instructed to take the morning of your procedure with a few sips of water.
- Don’t put on any lotion, cream, powder, makeup, perfume, or cologne.
- Remove all jewelry, including body piercings.
- Leave all valuables, such as credit cards and jewelry, at home.
- If you wear contact lenses, wear your glasses instead. If you don’t have glasses, bring a case for your contact lenses.
What to bring with you
- A list of the medications you take at home
- Your rescue inhaler (such as albuterol for asthma), if you have one
- A case for your glasses or contacts
- Your Health Care Proxy form, if you have completed one
During your procedure
You will get a mouth guard to wear over your teeth to protect them. If you wear dentures, you will take them out right before your procedure.You will lie on your back or left side for the procedure. Once you’re comfortable, you will get medication through your IV that will make you relaxed and sleepy.
First, your doctor will use an endoscope to look at the area that’s blocked. An endoscope is a flexible tube with a camera that goes through your mouth and esophagus. If your doctor sees that your esophagus is narrow, they may need to dilate (widen) it before the stent is placed. This is done with special balloons or soft, flexible, rubber tubes.
After your esophagus is ready, your doctor will insert and position the stent with the help of fluoroscopy (a real-time x-ray). After the stent is in the right position, they will remove the balloons or rubber tubes so only the stent is left in place.
After Your Procedure
When you wake up after your procedure, you will be in the Post-Anesthesia Care Unit (PACU). You will get oxygen through a thin tube that rests below your nose called a nasal cannula. A nurse will be monitoring your body temperature, pulse, blood pressure, and oxygen levels.You will stay in the PACU until you’re fully awake. Once you’re awake, your nurse will bring you something to drink. Your doctor will talk with you about your procedure before you leave the hospital.
Your nurse will teach you how to care for yourself at home before you leave the hospital.
Side effects
- You may feel discomfort in your chest after your stent is placed. This is usually described as a feeling of pressure or soreness.
- If you have pain, try taking a pain medication such as acetaminophen (Tylenol®). Your doctor may also prescribe other pain medication.
- For some people, the pain is severe. If pain medications don’t help, tell your doctor or nurse. You may need to stay in the hospital for pain relief.
- You may have a sore throat for up to 24 hours after your procedure. Try sucking on lozenges and drinking cool liquids to soothe your throat.
At home
You can go back to doing your normal activities (such as driving and going to work) 24 hours after your procedure.Follow the instructions below about eating and drinking during the first 2 days after your procedure.
- On the day of your stent placement, drink liquids. You can also have soup, oatmeal, or cream of wheat, but don’t eat any solid food.
- Don’t drink alcohol for 24 hours after your procedure.
- One day after your procedure, you can begin to eat soft foods.
- Two days after your procedure, you can eat solid foods.
Eating with a esophageal stent
Follow the instructions below for as long as your esophageal stent is in place.- When you resume your normal diet, eat small pieces of food. Always chew them well before swallowing.
- Drink liquid with your meals to help food pass through the stent. Carbonated drinks such as cola or ginger ale also help food pass through.
- Always eat in an upright (sitting) position. Gravity will help food pass through your esophagus and stent.
- You can swallow pills or capsules whole. Drink at least 4 ounces of water after swallowing them.
Preventing reflux
Reflux is a burning or full feeling pushing up from your stomach. Try the following things to prevent reflux.- Stay in a sitting position for at least 2 hours after each meal.
- Sleep with the head of your bed raised to 30 to 45 degrees. You can use a wedge to raise the head of your bed. You can also use blocks to raise your bedframe at the head end.
Call Your Doctor or Nurse if You Have:
- Chest pain that doesn’t get better with acetaminophen or the medication your doctor prescribed
- Difficulty or pain while swallowing that lasts for more than 1 day
- Pain, bloating, or hardness in your abdomen (belly)
- Back or shoulder pain
- Difficulty breathing
- Black or dark stools
- Weakness or feel faint
- Nausea or vomiting or if you vomit blood
- Chills
- A temperature of 101° F (38.3° C) or higher
- Any problem you didn’t expect
- Any questions or concerns
Potential problems
associated with your stent
Acid Reflux
This may be a problem, particularly if your stent needs to
be placed across the opening between the esophagus and
stomach. An antacid medication may be helpful (consult
your doctor regarding which one). Try not to sleep too flat.
Prop yourself up to a 30-45 angle. Try using pillows or a
bed wedge. Both can be placed between the mattress and
box spring to raise the head of your bed. If you continue
to experience problems, contact your healthcare team.
Pain
As the stent expands it can cause some pain in the
chest area, which normally subsides after 72 hours.
Painkillers should be helpful. However, if the pain persists
contact your healthcare team.
Persistent Swallowing Problems
If your ability to swallow does not improve despite
following the advice in this booklet, it may be because the
stent is not in the correct position or has moved. Contact
your healthcare team for advice. You should also seek
advice if swallowing food and beverages causes you to
cough, or if you experience any breathing difficulties, if
you are losing too much weight or become dehydrated.
Meal suggestions
Below are some suggestions of suitable foods and meal
ideas for once you have progressed to stage 3 of your diet.
This list is intended as a guide, and you may include other
food items that you can chew well enough to swallow
easily with your stent. Remember to chew all foods well
and eat small and frequent meals and snacks.
Pancakes/waffles softened with butter and syrup
Oatmeal, or other hot cereal made with whole milk and
sugar, honey, or maple syrup.
Soft fruit, for example ripe banana, apple or other fruit
sauce or stewed pears.
Thick and creamy yogurt.
Fruit juice.
Scrambled or poached eggs.
Cereal (e.g., Rice or Cocoa Krispies™ or Cheerios™)
Macaroni and cheese.
Tender or ground meat in gravy, for example shepard’s
pie, corned beef hash, chicken stew.
Boneless fish with butter, tartar sauce or mayonnaise.
Tender or ground meat or vegetable curry with rice.
Buttered noodles.
Shredded or ground turkey or roast beef served with
mashed potato with added butter, cream or cheese.
Soft, well cooked vegetables, such as carrots,
peas or spinach.Spaghetti with ground meat sauce.
Breakfast
Dinner
If you have trouble maintaining your weight:
Drink nutritional supplements or homemade milk shakes
as snacks / meal replacements.
Try adding ice cream, sherbets, sorbets to ready-made
supplements such as Nutra-shakes™, Ensure™ or Boost™.
If it is too sweet, dilute with whole milk or evaporated milk.
If you have pills to take, consider taking them with
calorie-containing beverages instead of water.For more ideas, speak to your healthcare team.
Baked potato (no skin) with butter and soft filling, such
cheese or cottage cheese.
Soup with added cream, cheese, skimmed milk powder
or tender meat.
Canned fruits.
Quiche or omelette made with cheese, spinach or other
cooked vegetables.
Tuna, egg, chicken or ham salad made with a lot of
mayonnaise or plain yogurt.
Pudding, rice pudding or custard.
Thick and creamy yogurt.
Ice cream, sherbet or sorbet.
Mousse.
Crème caramel or flan.
Milky drinks, for example, milky coffee, hot chocolate
or malted drink.
Plain, soft cake, such as sponge, angel food, or pound.
Frozen yogurt.

https://emedicine.medscape.com/article/1948973-overview#a2

No comments:
Post a Comment